A Guide to Modern NHS Facilities Management
- Craig Marston
- 17 hours ago
- 15 min read
When you think about what makes a modern NHS hospital work, it’s easy to focus on the surgeons, the nurses, and the life-saving equipment. But behind the scenes, there’s a complex, strategic operation that keeps the entire building safe, efficient, and compliant: facilities management.
This isn't just about fixing leaks or changing lightbulbs. NHS facilities management is the art and science of coordinating a healthcare building’s physical environment (Hard FM) with all the user-facing services that happen within it (Soft FM). It treats the facility as a single, complex system where every single component—from the backup generators to the cleaning schedules—has a direct impact on patient outcomes.
The Strategic Core of Modern Healthcare Operations

Think of it as the central nervous system of a hospital. It’s the strategic engine that connects every part of the building to the ultimate goal of delivering outstanding patient care.
This discipline is typically split into two deeply connected categories. Hard FM covers the tangible, structural bits of the building—the electrical systems, plumbing, ventilation, and fire safety infrastructure. In contrast, Soft FM includes the human-centric services that make the environment safe and functional, like infection control, catering, portering, and security.
The Interplay Between Hard and Soft FM
A modern NHS facility simply can't function if these two areas operate in separate silos. The relationship between them is direct and absolutely critical. For example, a meticulously maintained ventilation system (Hard FM) is fundamental to preventing the spread of airborne infections, which is a core mission for the infection control teams (Soft FM).
Likewise, a reliable power supply isn't just about keeping the lights on. It’s about ensuring that life-support machines and diagnostic equipment operate without a single blip, directly influencing patient safety. When managed together, they create a resilient environment that can handle the intense demands of 24/7 clinical care.
The scale of this is huge. The UK's public sector facilities management spend is projected to hit £27 billion in 2025, with the NHS being a major part of the £17.5 billion from wider public bodies. Discover more insights into the public sector FM market to get a sense of the scope.
An Orchestra of Expertise
Achieving this kind of operational harmony is a lot like conducting an orchestra. Every specialist has to perform their role perfectly while staying completely in sync with everyone else.
A truly effective NHS facility operates when its physical infrastructure, digital systems, and clinical services are managed as one cohesive unit. Neglecting one component inevitably compromises the others, impacting everything from patient flow to regulatory compliance.
Getting this right involves a diverse group of stakeholders, each with a critical role to play. The table below breaks down who does what, showing how their responsibilities fit together to create a safe and functional healthcare environment.
Key Stakeholders in NHS Facilities Management
Stakeholder Role | Primary Responsibilities | Key Focus Area |
|---|---|---|
Estates & Facilities Managers | Oversee all Hard and Soft FM services, manage budgets, ensure compliance, and lead strategic planning. | Holistic operational performance and regulatory adherence. |
IT & Infrastructure Specialists | Manage the digital backbone: structured cabling, Wi-Fi, server rooms, CCTV, and telecoms infrastructure. | Ensuring reliable and secure digital connectivity for clinical and operational systems. |
Clinical Staff (Nurses, Doctors) | Act as end-users, providing feedback on how the facility supports their ability to deliver care effectively. | Patient safety, workflow efficiency, and the functionality of the clinical environment. |
Infection Control Teams | Develop and enforce protocols to prevent the spread of infections, liaising with cleaning and maintenance teams. | Hygiene, sterilisation, and environmental safety. |
Health & Safety Officers | Monitor and enforce compliance with health and safety regulations, including fire safety and risk assessments. | Staff and patient safety, risk mitigation, and legislative compliance. |
Procurement & Contract Managers | Source and manage third-party suppliers for services like catering, security, and specialised maintenance. | Value for money, supplier performance, and contract adherence. |
Each of these roles is a vital piece of the puzzle. From the Estates Manager coordinating the overall strategy to the IT Specialist ensuring a ward's Wi-Fi is robust enough for digital patient records, their collaboration is what keeps the facility running.
This foundational understanding shows that every element, from a single power socket to a complex network cable, is an integral part of the patient care journey.
Mastering NHS Compliance and Technical Standards
Getting NHS facilities management right isn’t just about making things run smoothly; it’s about getting the compliance right first. It can feel like wading through a sea of acronyms and regulations, but every single standard is there for a reason: to keep patients, staff, and visitors safe.
These aren't just guidelines; they're the non-negotiable rulebooks. They dictate everything from the sterility of the air in an operating theatre to the security of the building itself. Getting this wrong simply isn't an option.
Decoding HTMs and HBNs
At the heart of it all are two critical sets of documents: Health Technical Memoranda (HTM) and Health Building Notes (HBN). Think of them as the official blueprints for creating and maintaining a healthcare facility that's truly fit for purpose. They provide the highly specific, technical guidance on how building systems should be installed, run, and looked after.
Health Technical Memoranda are the practical 'how-to' manuals. They dive into the nitty-gritty of specialised engineering, laying out best practices to stamp out risks. Take HTM 03-01, for example. It gives explicit instructions for ventilation, dictating precise air change rates in an operating theatre to control airborne germs and protect patients when they are at their most vulnerable.
Health Building Notes, on the other hand, come in at the design and planning stage. They are the go-to resource for new builds or major refurbishments, ensuring the physical layout and design of a building support modern clinical workflows right from the drawing board. Together, HTMs and HBNs provide a comprehensive library of standards that steer every phase of a building's life.
These standards are not merely suggestions; they are the bedrock of patient safety. A failure to adhere to an HTM for electrical systems or an HBN for ward design can have direct and serious consequences for patient care and organisational reputation.
The Role of the Care Quality Commission (CQC)
While the HTMs and HBNs spell out the technical 'what', the Care Quality Commission (CQC) is the independent regulator that checks if those standards are actually being met. The CQC’s job is to make sure health and social care services are providing people with safe, effective, compassionate, and high-quality care.
When the CQC inspects a facility, they look at everything. They’ll scrutinise maintenance logs for critical systems, assess cleaning and infection control procedures, and check that fire safety plans are solid. A poor CQC rating can have massive repercussions, which is why compliance is always front and centre for any NHS Trust. Understanding the intricate medical centre cleaning protocols and patient safety measures that underpin healthcare operations is a key piece of this puzzle.
Translating Standards into Action
Knowing the rulebooks is one thing, but actually putting them into practice is where the real work begins. This is where strategic NHS facilities management proves its worth, turning complex requirements into tangible, everyday actions.
Here’s what that looks like on the ground:
Infection Control: Following HTM 01-05 on decontamination in a dental practice ensures every instrument is sterilised correctly, stopping cross-infection in its tracks.
Water Safety: Applying the guidance in HTM 04-01 for managing Legionella in water systems is about protecting vulnerable patients from a dangerous, yet entirely preventable, illness.
Specialised Environments: In mental health facilities, the design itself is a crucial safety feature. For instance, correctly implementing enhancing patient safety with anti-ligature solutions in NHS hospital wards is a direct application of these safety-first design principles.
Ultimately, mastering these standards isn't about ticking boxes. It’s about deeply understanding the 'why' behind every rule to proactively build and maintain healthcare environments that are fundamentally safe, resilient, and ready to support the work of healing.
Navigating Procurement and Finding the Right Partners
Choosing the right contractors is one of the most critical decisions an NHS Trust will ever make for a facilities management project. The entire success of a new build, a complex relocation, or a major refurbishment often rests on the expertise and reliability of these partners. A well-run procurement process isn't just about finding the cheapest quote; it's about building a solid foundation of trust, compliance, and shared goals from day one.
The journey starts by working through the formal procurement routes designed for the public sector. These pathways are there for a reason—to ensure fairness, transparency, and genuine value for money. For many Trusts, this means looking beyond open tenders and using established frameworks instead.
Utilising Established Frameworks for Lower Risk
One of the smartest ways to de-risk a project is to use established procurement frameworks, like those offered by the Crown Commercial Service (CCS). Think of these as a pre-vetted list of suppliers who have already been put through the wringer—assessed for their financial stability, technical skill, and deep understanding of public sector needs.
Engaging suppliers through a CCS framework gives you several powerful advantages:
Reduced Administrative Burden: It slashes the time and internal resources needed for due diligence because the suppliers have already met tough criteria.
Ensured Compliance: All listed suppliers are confirmed to be compliant with public procurement regulations, which minimises legal and commercial headaches.
Competitive Pricing: The terms are often pre-negotiated, using the collective buying power of the public sector to secure better value.
This structured approach lets NHS facilities management teams concentrate on the specific needs of their project, confident they are choosing from a pool of capable and trustworthy partners.
The diagram below shows how these procurement frameworks, integrated FM, and SLAs all fit together at the heart of the process.
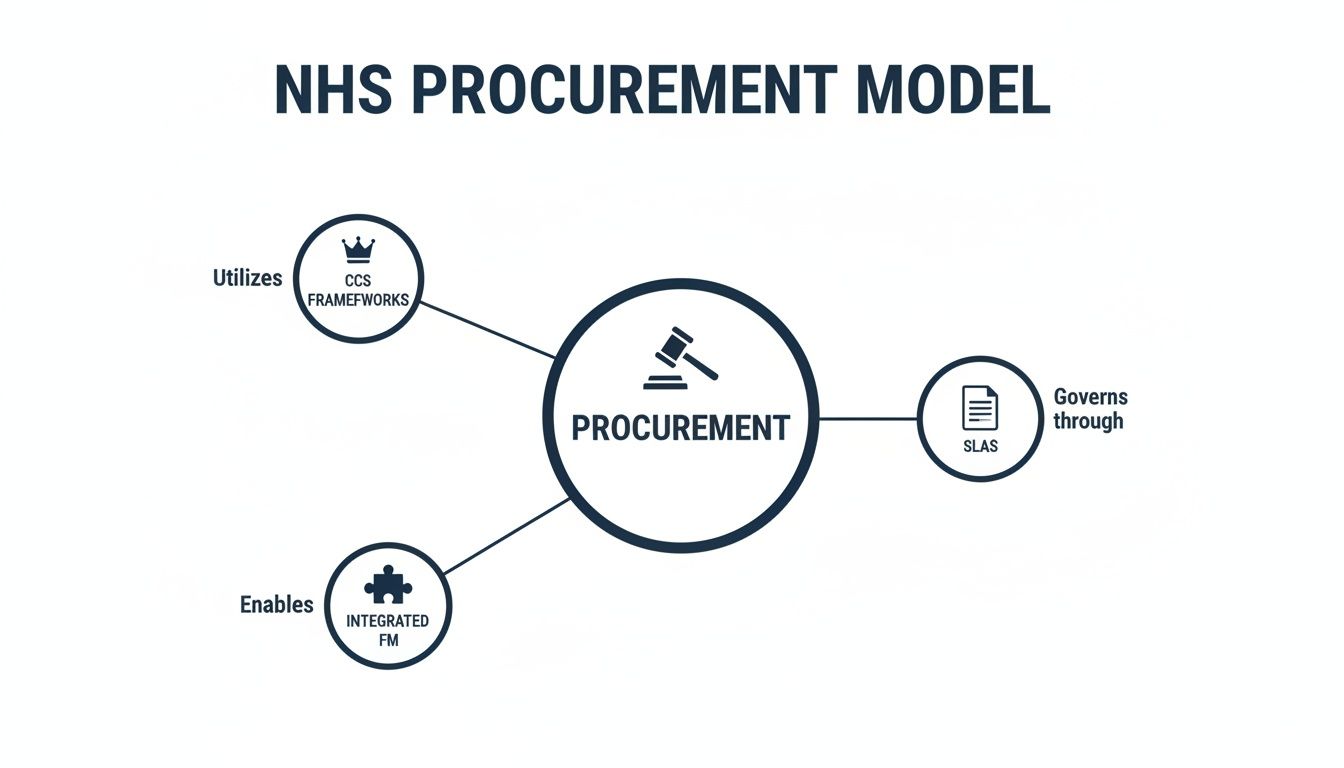
As this model shows, a robust procurement strategy not only gives you access to compliant partners but is also governed by clear, enforceable agreements.
Integrated FM vs Specialist Contracts
A core decision you'll face is whether to go for a single, all-in-one integrated facilities management contract or to hire individual specialists for different services. An integrated FM provider takes on all Hard and Soft FM services under one roof, giving you a single point of contact and accountability. This can really simplify contract management and lead to a more joined-up service.
However, for highly specialised projects—like a major data centre upgrade or the rollout of a new clinical IT system—bringing in specialist contractors is often the better move. This approach lets the Trust tap into deep, niche expertise for the most critical parts of the project, ensuring each element is handled by a dedicated expert.
Crafting Effective Service Level Agreements
No matter which contracting model you choose, the most vital tool for ensuring accountability is the Service Level Agreement (SLA). A well-written SLA goes far beyond vague promises and sets out precise, measurable performance indicators.
An SLA is more than a contract; it's a shared definition of success. It translates a Trust’s objectives for patient care and operational excellence into concrete performance metrics that vendors must meet.
For instance, instead of a contractor agreeing to "provide timely maintenance," a strong SLA will specify that "all Priority 1 electrical faults must be responded to within 15 minutes and resolved within one hour." It should also clearly spell out the consequences of failing to perform. This level of detail aligns vendor performance directly with the Trust’s mission, making sure every partner is contributing effectively to a safe and efficient healthcare environment.
Integrating IT: The Digital Backbone of Modern Healthcare

In a modern NHS facility, the IT infrastructure is no longer an afterthought—it’s as fundamental as the plumbing or the power grid. Treating digital systems as something to be tacked on later is a guaranteed recipe for operational failure. Today, everything from electronic patient records and diagnostic imaging to automated building controls depends on a robust, resilient, and secure network.
Think of it this way: a hospital's IT infrastructure is the digital equivalent of a city's road network. If the roads are narrow, poorly planned, and full of potholes, traffic grinds to a halt. In the same way, a poorly designed network creates digital bottlenecks that can delay access to critical patient information, disrupt clinical workflows, and ultimately compromise patient care.
Effective NHS facilities management demands that IT is woven into the very fabric of the building from the earliest design stages. This means planning for structured cabling pathways, resilient server rooms, and comprehensive Wi-Fi coverage is just as important as mapping out electrical circuits.
Building the Digital Foundation
The physical components of the IT network form the digital foundation of any healthcare facility. Getting this right isn't just about plugging in a few computers; it’s about building an entire ecosystem where data flows securely and reliably to where it's needed most.
This integrated approach is more critical than ever, especially with the immense pressure on existing infrastructure. By 2025, the NHS was already facing an £11.6 billion maintenance backlog in hard facilities, a figure that highlights years of underinvestment. We can't afford to make the same mistake with our digital systems.
Building a truly digital-first facility requires a strategic approach. It’s essential to plan for future technological demands, not just current needs. For a deeper dive, check out our practical guide on designing the modern NHS network, which offers more insights into future-proofing healthcare infrastructure.
Core Components of an Integrated IT System
A successful digital infrastructure is built on several interconnected pillars. Each must be planned and installed with precision to ensure the entire system functions as a cohesive whole, supporting both clinical and operational needs.
Structured Cabling: This is the physical superhighway for data, connecting everything from workstations and Wi-Fi points to critical medical equipment. Using high-grade cabling like Cat6a is vital for supporting high-bandwidth applications like medical imaging.
Resilient Wi-Fi: Wireless connectivity is no longer a convenience; it's essential for mobile clinical devices, patient communication, and staff workflows. A professional wireless survey is crucial to guarantee seamless coverage across the entire facility.
Secure Server Rooms: These are the heart of the digital operation, housing the systems that store and process patient data. They require dedicated power, cooling, and security measures to ensure 100% uptime.
Integrated Communications: Modern VoIP (Voice over Internet Protocol) telephone systems and audio-visual solutions for meeting rooms and training centres must be integrated directly into the core network for reliable performance.
Integrating systems like CCTV and access control onto the same unified network streamlines management and improves security. A single, well-managed infrastructure is far easier to secure and maintain than multiple, disparate systems.
The final pillar is the commercial electrical installation and certification that powers it all. Every data point, server rack, and network switch depends on a clean and reliable power supply. Electrical work in an NHS environment must be meticulously planned and certified to meet stringent safety and resilience standards, ensuring the digital backbone never fails. This synergy between power and data is the essence of modern, resilient healthcare infrastructure.
IT Infrastructure Checklist for NHS New Builds and Relocations
To bring all these elements together, a practical checklist is invaluable. It helps ensure that no critical digital component is overlooked during the planning and construction phases of a new build or a major relocation project. This isn't just about ticking boxes; it's about building a coherent, future-proof digital environment from the ground up.
Infrastructure Component | Key Consideration | Compliance Standard |
|---|---|---|
Structured Cabling | Plan pathways for Cat6a or higher to support future bandwidth needs. Ensure separation from power lines. | BS 6701, BS EN 50173 |
Wireless Network (Wi-Fi) | Conduct a predictive and on-site survey to guarantee full coverage for clinical and guest access. | NHS Wi-Fi Standards, HBN 00-10 |
Server/Comms Rooms | Design for resilient power (UPS, generator), dedicated cooling, and physical security (access control). | HTM 06-01, ISO 27001 |
IP Telephony (VoIP) | Ensure network is configured for Quality of Service (QoS) to prioritise voice traffic and prevent call drops. | HBN 14-01 |
CCTV & Access Control | Integrate onto the core IP network for centralised management and monitoring. | Data Protection Act 2018, CCTV Code of Practice |
Audiovisual (AV) Systems | Plan for integrated systems in meeting rooms, lecture theatres, and MDT rooms. | HBN 14-01 |
Electrical Infrastructure | Install dedicated, clean power circuits for all IT equipment, with appropriate certification. | BS 7671, HTM 06-01 |
Patient Entertainment Systems | Ensure cabling infrastructure supports IP-based systems at each bedside. | Relevant HBN/HTM guidance |
Using a structured checklist like this from day one keeps the project team aligned. It ensures that the digital infrastructure is treated as a core utility, fully integrated into the building's design, and compliant with all the necessary NHS and industry standards. This forward-thinking approach is what separates a truly modern healthcare facility from one that's already playing catch-up.
Ensuring a Smooth Handover and Long-Term Success

The final construction work might be complete, but the project is a long way from being over. The handover phase is that critical moment of transition, turning a building site into a living, breathing healthcare environment.
Without a meticulously planned handover, even the most state-of-the-art facility can stumble into operational chaos from day one. Get it wrong, and you risk undermining the entire investment.
A successful handover in NHS facilities management isn’t a single event. It's a carefully orchestrated process designed to bridge the gap between construction and operation, empowering the in-house FM team to take full ownership of their new space. It’s all about making sure that from the moment the doors open, every system works as intended and every member of staff knows exactly how to use the new facility safely and effectively.
The Pillars of an Effective Handover
A rock-solid handover process is built on three essential pillars: comprehensive documentation, thorough staff training, and meticulous asset management. Neglecting any one of these can create significant long-term headaches, from compliance breaches to eye-watering reactive maintenance bills.
Operation & Maintenance (O&M) Manuals: Think of these as the detailed instruction books for the building. They need to be comprehensive, easy to follow, and cover absolutely everything, from the complex HVAC system to the specialised medical gas pipelines. Digital, searchable O&M manuals are now the standard, giving teams instant access to critical information when they need it most.
Staff Training and Familiarisation: Just handing over a set of keys without proper training is setting your teams up to fail. You need dedicated sessions for both clinical and FM staff to get them comfortable with new systems, layouts, and safety protocols well before the facility goes live. This covers everything from operating the new access control system to knowing the fire evacuation routes like the back of their hand.
As-Built Drawings and Certification: The final drawings must reflect exactly what was built, showing the precise locations of all cabling, pipework, and structural elements. Alongside this, all commercial electrical installation and certification documents must be provided. This isn't just paperwork; it’s the proof of compliance that ensures all future maintenance can be done safely.
A seamless handover isn't just about transferring documents; it's about transferring knowledge. The goal is to equip the in-house team with the confidence and competence to manage the facility independently from day one.
Establishing Long-Term Reliability
Beyond that initial transfer of responsibility, the handover process really sets the stage for the building's entire operational lifecycle. This is where strategic asset management and ongoing support become absolutely vital.
Meticulous asset tagging is the foundation of any modern maintenance strategy. Every single piece of equipment, from a boiler in the plant room to a server rack in the comms room, should be tagged and logged in a Computer-Aided Facilities Management (CAFM) system. This creates a complete inventory, paving the way for planned preventative maintenance schedules and making it easy to track an asset's history. To nail this, it’s worth understanding the detailed steps involved; you can learn more about how to perform an asset audit in our comprehensive guide.
Finally, getting ongoing support contracts in place from the outset is crucial for protecting the investment. Specialised systems, particularly in IT and building management, require expert support that your in-house team might not have. Having these agreements in place before the handover ensures there's a clear escalation path for any issues, minimising potential downtime and ensuring the long-term reliability of the facility's most critical systems.
Unmanned Building Management in the NHS
The drive for efficiency in NHS facilities management has led to growing interest in autonomous buildings. These are spaces designed to operate securely and effectively with minimal or zero on-site staff, which can dramatically reduce operational costs and improve flexibility.
What Is Unmanned Building Management?
In practice, unmanned building management means creating a facility, or a dedicated unit within one, that can largely run itself through integrated technology. It's about automating core functions like access, security, and environmental controls so they work together seamlessly.
Imagine a satellite diagnostic clinic or a secure records archive. An authorised staff member could use their NFC-enabled phone or ID card to unlock the door. This single action could trigger a chain of events: the lights and heating in a specific zone turn on, the alarm system disarms, and a log is created for auditing purposes. Meanwhile, integrated CCTV and environmental sensors monitor the space, automatically flagging security breaches or equipment failures to a central management hub.
Why Many Unmanned Building Projects Fail
Many unmanned building projects stumble because they treat access control, power, and data as separate disciplines. This siloed approach is a recipe for failure. A common mistake is installing a state-of-the-art access system but connecting it to a standard, non-resilient network port. The first time there's a power outage or a network switch fails, the entire security system collapses, potentially locking staff out (or in) and creating a major security vulnerability.
The key takeaway is that access, power, and data must be designed together as a single, cohesive system. One cannot function reliably without the others. A door entry system is only as robust as the network that supports it, and that network is only as dependable as its power source.
True autonomous operation is only achieved when access control, power resilience (like UPS backups), and data connectivity are planned as one cohesive unit. A failure in one is a failure in all three.
Building Out a Fully Autonomous Unmanned Building Unit
Constructing a truly autonomous unit requires the careful integration of several key technologies. These systems must be planned from the ground up to ensure they are interdependent and resilient.
Access Control: Choosing the right lock technology is crucial. For maintenance and operational reasons, battery-less, NFC proximity locks are an excellent choice. They are powered by the user's phone or card upon contact, completely eliminating the significant operational burden of monitoring and replacing hundreds of batteries. This removes a common and critical point of failure in traditional systems.
Power and Data Backbone: This is the non-negotiable foundation. It involves robust structured cabling to connect all systems, supported by an uninterruptible power supply (UPS) and potentially a generator for long-term resilience. The commercial electrical installation and certification must be meticulously executed to HTM standards to ensure the system never fails when it's needed most.
Integrated Security: A modern, IP-based CCTV system integrated into the core network provides essential remote monitoring capabilities, allowing a central team to respond to incidents without needing to be on-site.
These systems are commonly used for remote diagnostic centres, administrative hubs, out-of-hours clinics, and secure storage facilities. They allow the NHS to expand its estate efficiently without the corresponding increase in staffing overheads, making them a cornerstone of modern, strategic NHS facilities management.
Planning a complex NHS infrastructure project requires specialist expertise in integrating IT, electrical, and security systems. At Constructive-IT, we provide end-to-end solutions that ensure your new build or relocation is compliant, resilient, and ready for the future. Contact us to discuss your project requirements.






Comments