A Guide to Modernising and Future-Proofing NHS Facilities
- Craig Marston
- Jan 17
- 16 min read
When you think of NHS facilities, the first image that probably comes to mind is a sprawling hospital. But that’s only a fraction of the story. The NHS estate is a vast, complex ecosystem of specialised treatment centres, community clinics, GP surgeries, and the critical administrative hubs that keep everything running. For the IT and facilities managers on the ground, this diverse and often ageing property portfolio presents a unique set of operational and technological headaches.
Understanding The Modern NHS Facilities Landscape

When the National Health Service was born back in 1948, it was one of the biggest public sector takeovers in British history. On the 5th of July, the service suddenly became the custodian of 1,143 voluntary hospitals and 1,545 municipal hospitals, stitching a fragmented collection of buildings into a single, unified organisation.
Today, that estate has grown into a sprawling network that looks completely different. The modern landscape of NHS facilities is no longer about a single, monolithic hospital. Instead, it’s a distributed model of care, where patient services are delivered across a huge range of specialised environments, including a growing number of unmanned or semi-autonomous sites.
The Diverse Ecosystem of NHS Properties
Managing this property portfolio means juggling an incredible variety of building types, ages, and purposes. Unsurprisingly, each one brings a distinct set of challenges for infrastructure modernisation and maintenance.
This varied ecosystem includes:
Acute Hospitals: These are the large, complex sites with operating theatres, A&E departments, and intensive care units. Here, infrastructure resilience isn't just a goal; it's an absolute necessity.
Community Health Clinics: Smaller, local centres offering services like district nursing, physiotherapy, and mental health support. They are often housed in older or repurposed buildings that were never designed for modern IT.
GP Surgeries: As the frontline of primary care, these practices need rock-solid connectivity for patient records, appointment systems, and the rise of digital consultations.
Specialised Treatment Centres: Facilities dedicated to specific fields like oncology, cardiology, or dental care. These are packed with highly specialised, data-hungry medical technology.
Administrative Hubs & Unmanned Units: The operational backbone of an NHS Trust, including a rising number of satellite offices, equipment stores, or on-call staff quarters that are not permanently staffed. In these buildings, remote management, security and reliable automation are paramount.
The core challenge for IT and facilities managers is trying to unify this incredibly diverse estate. A digital strategy that works perfectly for a brand-new hospital wing might be completely impractical for a listed community clinic, demanding a flexible and highly strategic approach to modernisation.
The Pressure on Legacy Infrastructure
Let's be honest, many of these facilities were built long before anyone could have imagined the demands of digital healthcare. The shift towards interconnected care, Electronic Patient Records (EPR), and medical IoT devices is placing immense pressure on the legacy infrastructure holding these buildings together.
Outdated cabling, insufficient power, and patchy Wi-Fi aren't just minor inconveniences; they create genuine risks to operational efficiency and patient safety. For the managers tasked with overseeing these properties, a forward-thinking infrastructure plan isn't merely an upgrade—it's the essential foundation for meeting the rigorous standards of modern healthcare and delivering the quality of care that patients expect and deserve.
The Rise of Unmanned Building Management

As NHS Trusts strive for greater efficiency, the concept of unmanned building management is moving from theory to reality. In practice, this means creating fully autonomous units—like satellite clinics, storage depots, or on-call staff facilities—that can operate securely and efficiently without permanent staff on site. This involves the centralisation of control over security, access, and environmental systems.
However, many unmanned building projects fail. The primary reason is a disconnected design approach. Teams often specify access control, CCTV, power systems, and data connectivity as separate, siloed elements. When these are not designed together as a single, cohesive system, the result is instability, security gaps, and operational chaos. For an unmanned facility to succeed, its digital nervous system must be flawlessly integrated.
The Holy Trinity: Access, Power, and Data
To build out a fully autonomous unmanned building unit, these three pillars must be designed in unison from day one:
Access Control: The system must be reliable and fail-safe. Battery-less, NFC proximity locks are a prime real-world example of the right technology choice. They eliminate the single most common failure point: dead batteries. Staff can use their existing ID cards, and access logs are created without depending on a fragile, battery-powered lock.
Power: The entire system needs a certified, resilient electrical installation with Uninterruptible Power Supply (UPS) backup. If the power fails, the building’s network and security systems must remain online. This is non-negotiable for maintaining security and remote oversight.
Data: A robust, dedicated data link is essential for remote management. This connection supports CCTV streams, access control logs, and remote diagnostics. Without reliable data, the facility is essentially blind and unmanageable.
These integrated systems are commonly used for community diagnostic centres, remote equipment stores, and secure drug dispensaries where controlled, auditable access is critical but permanent staffing is inefficient.
Operational and Maintenance Considerations
Managing an unmanned facility requires a shift in maintenance strategy. Instead of relying on on-site staff for daily checks, the focus moves to proactive remote monitoring and planned preventative maintenance. This includes remote diagnostics for network equipment, automated alerts for power failures, and a clear operational plan for responding to security breaches or system faults. Certified commercial electrical installation is not just a one-off task; regular testing and certification become crucial to ensuring ongoing safety and reliability in a building with no daily human oversight.
A well-designed network is also crucial for supporting modern IP-based CCTV systems. Comprehensive CCTV coverage provides not only security but also invaluable operational insight, allowing managers to remotely verify deliveries, check facility conditions, and ensure the safety of authorised personnel during their visits. This digital backbone connects every critical function, from a clinician accessing patient records in theatre to a facilities manager monitoring an unmanned storage unit from a central hub.
The integration of specialised healthcare safety software solutions is also vital for modernising these varied NHS facilities. These platforms rely entirely on the underlying network to track assets, manage compliance, and ensure a safe environment for everyone, whether the building is staffed or not.
A well-designed network in any clinical setting is invisible but indispensable. It works silently in the background, ensuring that a clinician’s focus remains entirely on the patient, not on a spinning loading wheel or a dropped connection. This same principle of invisible reliability is the key to a successful unmanned facility.
Ultimately, by linking specific technologies to both operational efficiency and patient safety, IT and facilities managers can build a powerful business case for investing in a robust, future-ready network. For more detailed insights, you can find a practical guide on designing the modern NHS network that explores these concepts further. This integrated approach ensures every part of the facility is equipped to meet the demands of modern healthcare.
Getting to Grips with NHS Compliance and Regulations
When you’re working on an NHS facility, compliance isn’t just another box to tick. It’s the absolute bedrock of patient safety, data security, and operational integrity. Every single cable you run and every server you install has to meet a web of stringent regulations. Get it wrong, and you’re not just looking at project delays and costly rework; you’re facing serious risks to patient care.
Navigating this landscape means getting familiar with the rulebooks that govern both the physical infrastructure and the digital systems running on it. These aren’t just friendly suggestions—they are mandatory requirements designed to make sure every NHS facility is safe, secure, and fit for modern healthcare. These rules dictate everything from the type of electrical sockets used near a patient's bed to the security protocols that lock down sensitive health records.
The Core Rulebooks for NHS Infrastructure
At the heart of it all are a few key documents that every facilities and IT manager should know inside and out. These aren’t high-level, theoretical guides; they provide practical, prescriptive instructions for designing and installing systems in a clinical setting.
Two of the most important ones you'll come across are:
Health Technical Memoranda (HTM): These are the go-to guides for the design, installation, and upkeep of specialised building and engineering tech in healthcare. For instance, HTM 06-01 is all about electrical services, spelling out the critical requirements for power resilience and safety in clinical areas.
Health Building Notes (HBN): These offer best-practice guidance for planning new healthcare buildings or adapting existing ones. HBNs influence everything from the physical layout of a ward to the specific requirements for a comms room that houses clinical data.
Getting your head around these documents from the very start is the first step to designing a project that’s compliant from day one. It’s the best way to prevent expensive surprises and last-minute changes down the line.
Protecting Patient Data Is Non-Negotiable
Beyond the bricks and mortar, the digital and data security side of things is absolutely paramount. The NHS handles some of the most sensitive personal information imaginable, and keeping it safe is both a legal and ethical duty. Two frameworks really drive this mission, shaping how every network and system is designed and managed.
The first is the NHS Data Security and Protection Toolkit (DSPT). This is an online self-assessment tool that lets organisations measure how they stack up against the National Data Guardian’s 10 data security standards. This isn't a one-and-done exercise; it’s an annual requirement that has to be baked into the very architecture of your network.
Security isn't an afterthought you can bolt on later. Principles from the DSPT and GDPR have to be woven into your network design from the outset. A truly secure network is built on foundations like strict access control, end-to-end encryption, and logical segmentation to protect patient data at every single point.
This means that from the moment a new network is even on the drawing board, data protection has to be front and centre. We’re talking about physical security for server rooms, logical access controls on the network itself, and robust encryption for data whether it’s sitting on a server or flying across the network.
Physical Security and Access Control
Compliance doesn't stop at the digital gate; it extends right down to the physical security of your critical infrastructure. Server rooms and communication closets in NHS facilities aren't just IT spaces—they are secure zones protecting the digital lifeblood of the hospital.
The standards get very specific here, covering everything from fire suppression and environmental monitoring to solid access control. Only authorised personnel should ever be able to physically get to your core network equipment. This prevents tampering, theft, or unauthorised connections and is a critical part of both the DSPT and wider security best practices.
We’ve put together a quick table to summarise the key standards and what they mean for your infrastructure planning.
Key NHS Infrastructure Standards and Their Focus Areas
This table breaks down some of the most important regulations and standards, highlighting what they cover and how they directly impact the IT and electrical infrastructure you'll be installing.
Standard/Regulation | Primary Focus Area | Practical Implication for Infrastructure |
|---|---|---|
Health Technical Memoranda (HTM) | Specialised building and engineering services. | Dictates requirements for electrical resilience (e.g., UPS, generators), medical gases, and ventilation in critical areas. |
Health Building Notes (HBN) | Design and planning of healthcare facilities. | Influences the layout, size, and environmental controls for server rooms, comms closets, and clinical IT workspaces. |
NHS Data Security (DSPT) | Protection of sensitive patient information. | Mandates network segmentation, access controls, and encryption. Requires secure physical housing for network hardware. |
BS 7671 (IET Wiring Regulations) | Electrical installation safety in the UK. | Governs all electrical wiring, including power to comms racks, outlets, and ensuring separation from data cabling. |
General Data Protection (GDPR) | Legal framework for data protection and privacy. | Enforces "privacy by design," meaning security must be built into network architecture from the start, not added on. |
By integrating these regulatory demands into your project plan from the very beginning, you ensure your facility not only meets the highest standards of patient care but is also built to be resilient against the threats of today and tomorrow.
Building the Four Pillars of Future-Proof Infrastructure
A resilient NHS facility doesn’t just happen by accident; it's meticulously engineered from the ground up. Its real strength rests on four interconnected pillars of infrastructure that absolutely must be designed and delivered as a single, cohesive system. When these critical elements are planned in isolation, you’re just creating performance bottlenecks, operational friction, and a whole host of future vulnerabilities.
There's only one way to build an environment that’s truly ready for the future: an integrated approach. By thinking about structured cabling, network design, server room integrity, and electrical systems all at once, you create a foundation that is not only robust and reliable today but is also primed to support the next wave of healthcare technology tomorrow.
Pillar 1: Warrantied Structured Cabling
Think of structured cabling as the hidden circulatory system of your entire facility. It’s the physical bedrock that every single digital interaction relies on, from a clinician accessing patient records on a computer to a CCTV camera streaming live video. In NHS facilities, opting for a high-quality, warrantied system like Excel Cat6A or fibre isn’t an expense—it’s a long-term investment in pure reliability.
A 25-year manufacturer's warranty gives you more than just peace of mind; it’s a guarantee of performance that will last for decades. This ensures your cabling can handle the ever-increasing data loads from medical imaging, IoT devices, and future technologies without needing a costly and disruptive overhaul down the line. It's the first and most critical building block of a dependable digital estate.
Pillar 2: Intelligent LAN, WAN, and Wi-Fi Design
With that cabling foundation firmly in place, the next pillar is the active network that brings it all to life. A well-designed Local Area Network (LAN), Wide Area Network (WAN), and Wi-Fi system ensures that connectivity is seamless across every single corner of your complex site. This is about far more than just scattering a few wireless access points around and hoping for the best.
Professional Wi-Fi site surveys are essential to properly map out coverage, identify potential sources of interference, and guarantee consistent performance for critical mobile devices like Workstations on Wheels (WoWs). The design has to account for the unique construction materials and layouts of different buildings, ensuring clinicians and staff have reliable access wherever their work takes them.
Pillar 3: Resilient Server Rooms and Data Centres
Your server room or data centre is the beating heart of your facility's digital operations. It houses the critical systems that manage patient data, run clinical applications, and support the day-to-day administrative workload. Making sure it stays online requires a meticulous approach to its environment and security.
This boils down to a few key considerations:
Power Redundancy: Having Uninterruptible Power Supplies (UPS) and backup generators isn't optional; it's non-negotiable for maintaining operations during an electrical disruption.
Environmental Controls: Precise cooling and humidity control are vital to prevent hardware from failing and to extend the life of your expensive equipment.
Physical Security: Robust access control, surveillance, and fire suppression systems are needed to protect these critical assets from unauthorised access and physical threats. Getting security right is essential, and for some environments, you may need to consider specialised fittings like those we cover in our guide to enhancing patient safety with anti-ligature solutions.
A server room isn't just a storage closet for technology; it's a controlled environment engineered for maximum uptime. Its design directly impacts the resilience of the entire facility's clinical and operational functions.
Pillar 4: Certified Power and Electrical Systems
The final pillar is the one that powers everything else: a certified, professionally installed electrical system. In a healthcare setting, this goes far beyond standard commercial wiring. It’s about creating a resilient power infrastructure that can support both general and life-critical systems without ever failing.
A certified electrical installation ensures that all work complies with rigorous standards like BS 7671 and the specific Health Technical Memoranda (HTM) for healthcare environments. This obsessive attention to detail prevents electrical interference with sensitive medical equipment and guarantees that backup power systems kick in seamlessly when needed, ensuring clinical continuity remains completely unbroken.
The sheer financial and operational scale of the NHS highlights why this level of infrastructure resilience is so vital. In 2022/23, NHS England received a total allocation of £152.6 billion, with £107.8 billion passed to integrated care boards. This huge budget has to support not only clinical services but also the constant maintenance and upgrading of the physical facilities that make them possible. By treating these four pillars as an integrated whole, you ensure every pound invested in infrastructure delivers maximum long-term value and performance for your NHS facilities.
A Proven Workflow for NHS Infrastructure Projects
Taking a complex infrastructure project from a blueprint to a fully operational reality inside a live clinical setting is a monumental task. Without a structured, proven workflow, projects can easily spiral out of control, leading to blown budgets, missed deadlines, and unacceptable disruption to patient care. A methodical, phased approach isn't just good practice; it's essential for navigating the unique challenges of modernising NHS facilities.
The journey doesn’t start with pulling cables. It begins with deep consultation and collaborative design. This first phase is all about getting the right people in a room—clinical leads, IT managers, estates teams, and department heads—to build a complete picture of what’s needed. It's about truly understanding clinical workflows, thinking ahead to future technology needs, and designing an infrastructure that can support both.
Designing for Long-Term Value and Performance
Once the requirements are crystal clear, the focus shifts to designing a system that delivers immediate performance and long-term value. This means looking beyond the initial project and making smart procurement decisions that will pay for themselves for decades to come.
A key strategy here is specifying systems that come with extensive, manufacturer-backed warranties. For instance, choosing a structured cabling system with a 25-year warranty isn't just about getting a piece of paper; it’s a guarantee of performance and a safeguard against future degradation. It ensures the physical layer can support multiple generations of network hardware.
An effective project workflow is built on a simple principle: meticulous planning minimises disruption. By investing time in detailed design, stakeholder collaboration, and rigorous pre-installation checks, you can de-risk the entire project and ensure clinical continuity is never compromised.
This forward-thinking approach is critical, especially as models of care evolve. Modern NHS facilities have seen huge shifts, with consultant-led bed numbers in England halving since the mid-1990s. This reflects a move towards more efficient, technology-driven healthcare, which in turn places even greater demands on the underlying infrastructure.
The process flow below shows the core infrastructure pillars—cabling, network, data centre, and power—that must be expertly managed within this workflow.
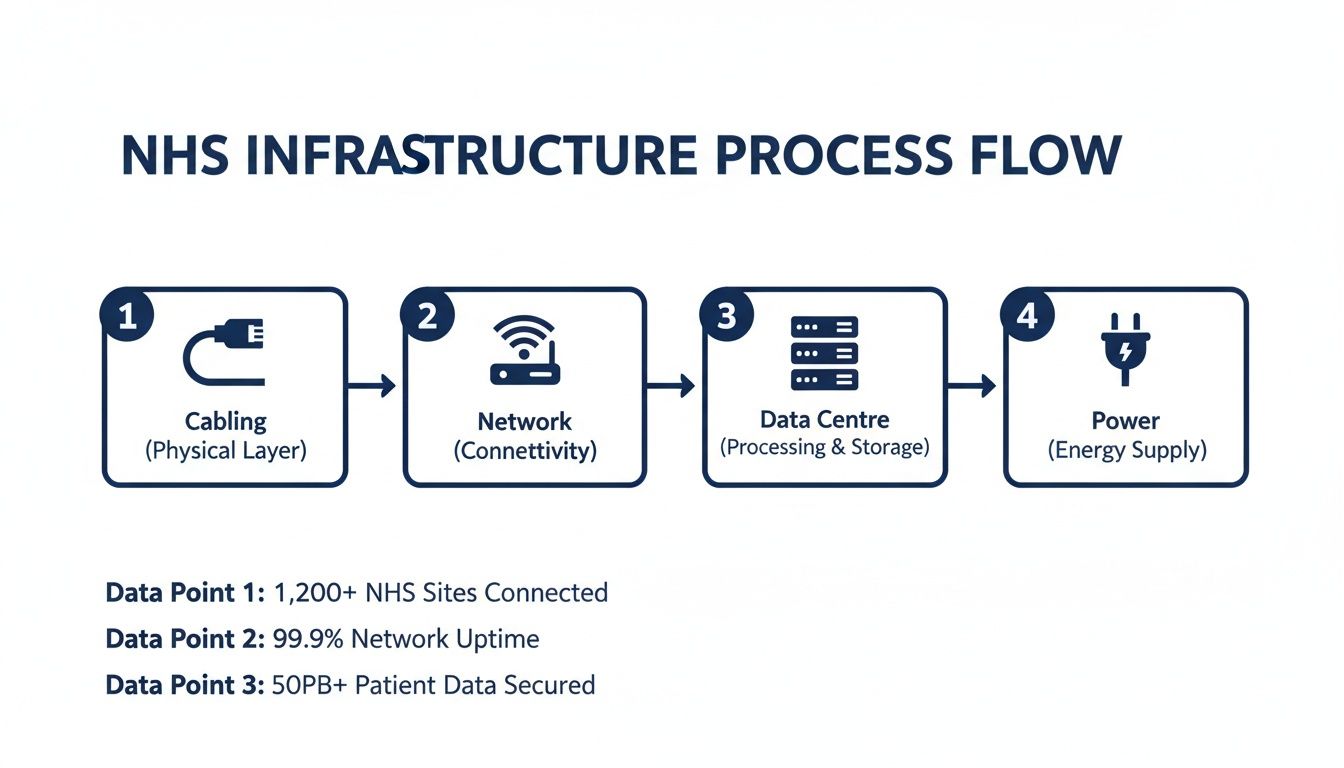
This visual highlights how each pillar is an interconnected stage in a successful project, demanding coordinated planning and execution from start to finish.
Execution and Go-Live Support
With a robust design signed off, the project moves into the execution phase. This is where disciplined project management is absolutely paramount. Minimising disruption in a live clinical environment requires careful scheduling, clear communication with staff, and phased rollouts that avoid impacting patient-facing services. You can see a real-world example of this in action in the NHS Highland Portree Dental Clinic project.
Before any system goes live, it has to pass rigorous testing and certification to ensure it meets the specified performance standards. This step is non-negotiable. It verifies that every single component is installed correctly and is ready to handle the intense demands of a busy clinical environment.
Finally, the workflow wraps up with dedicated on-site support during the critical "go-live" period. Having engineers present as new systems are switched on provides immediate assistance, sorts out any teething issues on the spot, and gives clinical and IT staff the confidence that the new infrastructure is ready for action. To get a better handle on this crucial stage, check out our guide on mastering IT infrastructure project management strategies.
Ensuring Clinical Continuity During Major Upgrades
In any NHS facility, whether it's a bustling acute hospital or a local community clinic, downtime isn't just an inconvenience—it's a direct risk to patient care. This makes the single most important goal of any infrastructure project maintaining absolute clinical continuity. Every upgrade, no matter how big, has to be carried out without interrupting the life-critical services that patients and staff rely on, second by second.
This calls for a risk mitigation strategy that goes far beyond a standard project plan. It demands a deep, practical understanding of a live healthcare environment, where meticulous planning is the only way to safeguard patients. A partner with proven experience in NHS facilities doesn't just manage the tech; they anticipate the unique challenges of working around active clinical workflows.
Phased Rollouts and Redundant Systems
The heart of a successful strategy is breaking the work down into carefully managed, phased rollouts to minimise disruption. Instead of a risky "big bang" approach, the project is segmented into manageable chunks. This could mean upgrading a single ward or department at a time, ensuring the rest of the hospital remains completely operational.
Another critical technique is building in redundancy before the old infrastructure is ever touched. By creating parallel network paths for essential systems, you create a safety net. This often involves:
Implementing Temporary Networks: Setting up parallel connectivity to keep vital services online while the primary network is being worked on.
Leveraging Robust Backup Power: Ensuring solid Uninterruptible Power Supply (UPS) systems and generators are ready to cover any potential electrical hiccups during a switchover.
A comprehensive risk mitigation plan isn't just a document; it's a commitment to patient safety. It is built on proactive communication, meticulous scheduling, and redundant technical solutions designed to make the transition completely seamless from a clinical perspective.
Communication and Scheduling
Of course, technical solutions alone are never enough. The human element is just as crucial. A detailed communication plan, developed in close partnership with clinical leads and department heads, is non-negotiable. This ensures all staff know exactly when and where work is happening, allowing them to adjust their workflows without any surprises.
Scheduling is everything. Any potentially disruptive work—like major power downs or core network switchovers—is fundamentally planned for outside of peak patient hours. This often means working overnight or on weekends to avoid any impact on scheduled appointments, surgeries, or A&E. It’s this deep respect for the clinical environment that separates a standard contractor from a true NHS infrastructure partner.
Answering Your Questions on NHS Infrastructure Projects
Embarking on a major infrastructure project within an NHS facility is a complex job, and it’s natural for IT and facilities managers to have questions. Let's tackle some of the most common ones we hear, helping you move forward with your project confidently.
How Can We Upgrade Without Disrupting Patient Care?
This is, without a doubt, the most critical question on the table. The solution isn’t a single trick but a combination of meticulous planning and a carefully phased rollout. All non-essential work has to be scheduled outside of clinical hours—that means overnight shifts and weekend work are standard practice to keep disruption to an absolute minimum.
For the systems that simply can’t go down, we build temporary or parallel networks. This strategy allows us to construct and thoroughly test the new infrastructure behind the scenes while the existing system keeps running. When it’s time to go live, the switchover is seamless, ensuring zero downtime for critical clinical services. Throughout this entire process, clear and constant communication with department heads is non-negotiable; it’s the only way to manage expectations and coordinate effectively.
What's More Important: Fibre or High-Spec Copper Cabling?
This isn't an either/or debate; it’s about applying the right tool for the right part of the job. Think of fibre optic cabling as the motorway of your network. It’s absolutely essential for the high-speed backbone connecting your buildings, floors, and comms rooms. Its massive bandwidth and ability to cover long distances make it the only real choice for these core links.
High-specification copper, like Cat6A, is more like the B-roads that lead right to the final destination—the wall outlets, wireless access points, and user devices. It provides more than enough bandwidth for today's devices and those coming down the line, and it's far more cost-effective for these shorter, final runs. The best networks are always a hybrid, structured design that uses both intelligently.
The most effective infrastructure designs are hybrids, leveraging fibre for the core network 'motorways' and high-performance copper for the final 'B-roads' to user devices. This creates a powerful, balanced, and cost-efficient network ready for future demands.
How Do We Actually Future-Proof Our Investment?
Future-proofing isn't about gazing into a crystal ball. It’s about building in headroom and sticking rigidly to established standards. The secret is to invest in a quality foundation that can adapt to whatever comes next.
Specify Warrantied Systems: Always opt for structured cabling systems that come with a 25-year manufacturer's warranty. This is your guarantee of performance and protects your investment for a generation.
Build in Headroom: Don't just design for today's needs. Install cabling and network hardware that go well beyond your current requirements. This gives you the capacity to handle future tech like advanced medical IoT devices and higher-bandwidth imaging without starting from scratch.
Adhere to Standards: Strict compliance with standards like HTM, HBN, and BS 7671 is non-negotiable. It ensures your infrastructure is robust, safe, and will be interoperable with the systems of tomorrow.
By focusing on a high-quality, standards-compliant foundation from day one, you build an infrastructure that can evolve alongside medical technology, avoiding the need for constant, disruptive, and expensive overhauls.
Planning and delivering a major infrastructure project in an NHS facility requires a deep understanding of technology, compliance, and the unique rhythm of clinical workflows. From fully staffed acute hospitals to complex unmanned units, ensuring reliability and security is paramount. If you're looking to modernise your facilities with a partner who understands these unique challenges, our team has the proven experience to guide you. Schedule a consultation with our experts today to ensure your next project is delivered safely, on time, and without compromising patient care.


Comments