A Practical Guide to Facilities Management in the NHS
- Craig Marston
- 2 days ago
- 17 min read
Facilities management in the NHS is the critical engine that powers patient care. It’s the complex web of services that has to run flawlessly in the background, ensuring hospitals and clinics are safe, compliant, and efficient enough to deliver clinical excellence.
When it’s done right, it directly impacts patient outcomes and staff productivity. From keeping life-saving equipment online to guaranteeing a sterile environment, effective facilities management in the NHS is the bedrock of modern healthcare.
The Foundations of NHS Estate Operations

Think of an NHS hospital as more than just bricks and mortar; it’s a highly complex ecosystem where every single component has to work in perfect harmony. At its heart, facilities management is the discipline that orchestrates this harmony, making sure the physical environment can support the relentless demands of clinical services.
It's the silent, essential work that keeps the lights on, the air clean, and critical systems running 24/7. The field is typically broken down into two distinct but deeply interconnected pillars. Getting your head around these is key to understanding the sheer scope of the job.
Hard FM: The Building's Core Systems
Hard Facilities Management (Hard FM) is all about the physical fabric of the building. These are the tangible, structural components that a hospital simply cannot function without.
Key responsibilities within Hard FM include:
Mechanical and Electrical Systems: This covers everything from the sophisticated HVAC (Heating, Ventilation, and Air Conditioning) systems controlling air quality in operating theatres to the electrical infrastructure powering life-support machines.
Plumbing and Drainage: Ensuring a constant supply of safe, clean water and managing waste systems to prevent contamination and uphold hygiene standards is non-negotiable.
Building Fabric Maintenance: This is the structural integrity of the building itself—roofing, walls, and flooring—which is vital for patient safety and infection control.
Fire Safety Systems: Maintaining alarms, sprinklers, and emergency lighting to protect patients, staff, and visitors if the worst should happen.
These elements aren't just 'nice-to-haves'; they are governed by incredibly strict regulations to ensure the safety and wellbeing of everyone in the building.
In the high-stakes NHS environment, a failure in Hard FM is never just an inconvenience. A power outage or ventilation failure can have immediate and severe consequences for patient care, highlighting the immense pressure on these services.
Soft FM: Services Supporting Patient Care
While Hard FM keeps the building standing, Soft Facilities Management (Soft FM) covers the services that make it a functional, safe, and welcoming place for people. These services are what turn a clinical building into a healing environment, supporting both patient recovery and staff efficiency.
Common Soft FM services in an NHS setting include:
Specialised Cleaning and Sterilisation: Adhering to rigorous infection prevention and control (IPC) protocols to minimise the spread of healthcare-associated infections (HAIs).
Security Services: Managing access control, monitoring CCTV, and ensuring the physical security of the site to protect vulnerable patients and valuable medical equipment.
Catering: Providing nutritious, diet-specific meals for patients is a key component of the recovery process.
Waste Management: Handling clinical and general waste safely and in full compliance with environmental regulations.
Successfully integrating both Hard and Soft FM requires specialist expertise, especially when you're navigating the significant maintenance backlogs and stringent regulatory demands so common in the NHS. For a deeper dive into this challenge, our guide to modernising and future-proofing NHS facilities is a valuable resource.
Navigating NHS Standards and Regulatory Compliance

Any project inside an NHS facility lives or dies by its ability to meet the trust’s incredibly high safety and operational standards. It might look like a mountain of red tape, but this regulatory framework is what keeps patients safe, protects staff, and ensures clinical services can run without a hitch.
Getting your head around these rules isn't just a box-ticking exercise; it’s the very foundation of building a resilient and effective healthcare environment.
At the heart of it all are the Health Technical Memoranda (HTMs). Think of these as the definitive instruction manuals for the design, installation, and upkeep of all the specialist engineering and building tech used in healthcare. They’re the blueprints for getting it right.
These aren't gentle suggestions. From the ventilation in an operating theatre to the backup power for life-support machines, HTMs are the yardstick that all facilities work is measured against. They turn high-level policy into practical, on-the-ground reality.
The Role of HTMs and IPC in Project Design
HTMs don't exist in a vacuum. They are designed to work hand-in-glove with Infection Prevention and Control (IPC) guidelines. IPC is all about stopping patients from picking up infections while in care, and the physical environment is a massive piece of that puzzle.
For example, an HTM will tell you the exact type of air filtration needed for an isolation ward. The IPC rules will then dictate the cleaning protocols for that same space. The two are completely intertwined. For facilities and IT teams, this means every single decision has to be seen through a compliance lens.
This has a direct impact on infrastructure projects. When you're running new data cabling, you have to think about how the trunking and outlets can be cleaned effectively to meet IPC standards. Likewise, any electrical work must follow HTM 06-01 to the letter, making sure power to critical areas is failsafe.
Below is a quick overview of the key frameworks you'll encounter and what they mean for your projects.
Key NHS Regulatory Frameworks for FM Projects
Framework/Standard | Governs | Practical Implication for IT/FM Teams |
|---|---|---|
Health Technical Memoranda (HTMs) | Design, installation, and maintenance of specialised building and engineering services. | Your go-to guide for everything. HTM 06-01 for electrical and HTM 02-01 for medical gas are essential reading for infrastructure work. |
Health Building Notes (HBNs) | Best practice guidance on the layout and design of new healthcare buildings and departments. | Informs the physical space requirements for IT rooms, comms cabinets, and user-facing technology during new builds or major refurbishments. |
Infection Prevention & Control (IPC) | Measures to prevent the spread of infections within healthcare settings. | All installed hardware (cabling, outlets, cabinets) must be easily cleanable. Surface materials and placement are critical considerations. |
NHS Estates Guidance | Overarching policies on estate management, sustainability, and efficiency. | Drives the need for energy-efficient network equipment, smart building tech, and sustainable design choices to meet net-zero targets. |
These frameworks aren't just separate documents; they form an interconnected system. A successful project manager knows how to navigate them all to deliver a solution that is safe, effective, and compliant from day one.
Meeting Sustainability and Energy Mandates
Beyond the immediate concerns of patient safety, the NHS is under immense pressure to become more sustainable and efficient. This isn't just about being green; it's a critical financial necessity.
The goal is to create healthcare facilities that are not only safe and effective but also sustainable and cost-efficient to run. This includes meeting ambitious government targets for achieving net-zero carbon emissions and improving the overall energy performance of the NHS estate.
This challenge is made even tougher by the sheer scale of the maintenance backlog. In the UK's National Health Service (NHS), facilities management is dealing with a staggering maintenance backlog that has climbed to £13.8 billion as of the 2023/24 Estates Return Information Collection by NHS Digital. To put that in perspective, that’s more than the entire £13.6 billion annual cost of running the whole NHS estate.
This figure highlights the incredible pressure on hard facilities management services, which cover everything from MEP systems to HVAC. These hard services are the dominant force in the UK facility management market, taking a 60.12% share in 2025, largely driven by the NHS crisis and the urgent need for EPC upgrades, where 28% of commercial properties are still rated D or lower.
For facilities managers, this boils down to a few key missions:
Improving Energy Performance Certificate (EPC) ratings by upgrading insulation, lighting, and HVAC systems.
Integrating renewable energy sources wherever possible to cut reliance on the national grid.
Choosing energy-efficient equipment for every new installation, from network switches to cooling units in server rooms.
A crucial part of health and safety also involves managing hazardous materials safely. This means getting to grips with current GHS and SDS compliance guidelines, which are essential in any healthcare facility. By embedding all these compliance and sustainability goals right from the planning stage, you build your project on a solid foundation of safety, resilience, and long-term value.
Making Procurement Work for Your NHS Project
Let’s be honest: procuring specialist services for an NHS project can feel like you’re trying to navigate a maze in the dark. The traditional open tender process is notoriously slow, eats up internal resources, and is often riddled with risk. The good news? Established procurement frameworks are designed to turn this challenge into a strategic advantage, giving you a direct, pre-approved route to suppliers who know exactly what they’re doing.
For facilities management in the NHS, these frameworks are more than just a convenient shortcut. They are essential tools for ensuring every pound of public money is well spent and for taking the risk out of critical projects. Think of them as a pre-vetted catalogue of trusted partners who have already proven their capability, financial stability, and deep understanding of the unique demands of a healthcare environment.
This approach saves an incredible amount of time and frees up your team to focus on the project itself, rather than getting bogged down in endless supplier vetting. It’s a structured, transparent, and efficient way to get the right expertise on board for your most important infrastructure work.
The Go-To Frameworks for NHS Infrastructure
When you’re looking to source partners for complex IT and facilities projects, a couple of frameworks really stand out for the NHS. They’re specifically designed to cut through the red tape while guaranteeing that every supplier meets the rigorous standards expected in a clinical setting.
These are your primary routes for securing specialist services:
Crown Commercial Service (CCS) Frameworks: As the UK's biggest public procurement body, CCS offers a whole range of agreements. Frameworks like RM6232 (Building Materials and Equipment) are fantastic for sourcing everything from network cabling and hardware to electrical components, all while ensuring competitive pricing and compliant products.
NHS-Specific Frameworks: Agreements like the Hard Facilities Management 2 (Hard FM 2) framework are built from the ground up for the health service. They give you a direct line to suppliers who are not just technically skilled but also fluent in the language of HTMs, IPC, and the day-to-day operational realities of an NHS trust.
Using these frameworks massively de-risks the whole process. Every single supplier listed has already been put through a tough evaluation, so you can move forward with confidence, knowing you’re engaging with credible, highly capable organisations.
How Frameworks Deliver Real-World Value
The benefits of using procurement frameworks go way beyond just being efficient. They are a central part of modern public sector strategy, designed to drive better outcomes and deliver tangible savings. They foster a competitive environment that ensures trusts get the absolute maximum value from their investments.
Outsourcing through these channels is a clear trend. In UK NHS facilities management, outsourced models are on track to capture 63.85% of the market in 2025, with a projected 2.77% annual growth through to 2031. This shift is being driven by public sector frameworks like the Crown Commercial Service’s RM6232, worth up to £35 billion, and NHS-specific contracts like Hard FM 2, which can slash costs by 10% compared to keeping it all in-house. With government procurement injecting £16.5 billion a year, these frameworks are empowering integrators to deliver comprehensive, bundled solutions. You can dig into the details in a market intelligence report on the NHS estates landscape.
By using frameworks, NHS trusts can sidestep the uncertainty of an open tender and plug directly into a pool of specialists who are already aligned with public sector values and compliance needs. It speeds up project timelines and dramatically increases the chances of a successful outcome.
At the end of the day, these frameworks change procurement from a bureaucratic headache into a powerful strategic tool. They provide a clear, compliant, and cost-effective roadmap for bringing in the specialist partners you need to build, maintain, and modernise the critical infrastructure that underpins patient care across the NHS.
Designing Resilient IT and Network Infrastructure
Modern healthcare doesn't just use technology; it runs on it. The IT and network infrastructure is the digital life support for any NHS facility, and getting the design right isn't an option—it's a clinical necessity. A network outage is no longer a simple inconvenience; it's a direct risk to patient care.
This digital backbone underpins everything from Electronic Health Records (EHR) and diagnostic imaging to the life-sustaining medical devices on the wards. Building it correctly means laying a foundation that is secure, scalable, and relentlessly reliable. The goal is simple: clinical services must operate without a hitch, 24/7.
The Non-Negotiable Core Components
A resilient network starts with its physical layer. This is absolutely not the place to cut corners, because the quality of the cabling and connections dictates the performance and longevity of the entire system. Think of it as the building's central nervous system—it has to be flawless from day one.
Two technologies form the bedrock of any modern NHS network:
Warranted Structured Cabling (Cat6/6a and Fibre): This is the high-speed data motorway connecting every device and system. Using high-quality, warrantied cabling like Excel Cat6 or fibre optic ensures consistent performance and future-proofs the installation against the ever-increasing demand for bandwidth. A 25-year warranty isn't just a marketing promise; it's a concrete assurance of long-term reliability.
Robust Wi-Fi Networks: In a clinical setting, wireless connectivity is mission-critical. A well-designed Wi-Fi network has to provide secure, high-speed access for clinical staff on the move, while also offering a completely separate and safe guest network for patients and visitors. This demands meticulous Wi-Fi surveying and planning to stamp out dead zones and ensure seamless roaming.
These core elements need to be planned with one eye on today's needs and the other firmly on the future. The explosion of IoT medical devices and the expansion of telemedicine services are coming, and the network needs to be ready.
Protecting Data in Secure Server Rooms
The server room is the beating heart of your IT infrastructure. It's where sensitive patient data is stored, processed, and managed, making its physical design and security absolutely paramount. An NHS server room is so much more than a locked cupboard with a few racks; it's a highly controlled environment engineered for maximum uptime.
Key design considerations include:
Physical Security: Robust access control, CCTV monitoring, and secure enclosures are your first line of defence.
Environmental Controls: Precise temperature and humidity management via dedicated cooling systems is essential to prevent hardware failure and extend the life of your equipment.
Power Redundancy: Uninterruptible Power Supplies (UPS) and backup generator connections are non-negotiable. They keep systems online during a power cut, ensuring clinical services continue.
Fire Suppression: You need specialised fire suppression systems that protect sensitive electronics without destroying them. It’s a must-have to safeguard critical infrastructure.
These measures all work together, creating a secure and stable environment where the digital heart of the hospital can beat without interruption.
When it comes to facilities management NHS, the server room is a critical asset where Hard FM and IT responsibilities meet. The physical security, power, and cooling are every bit as important as the network switches and servers they protect.
Integrating Essential Support Systems
A truly resilient infrastructure doesn't stop at data cables and servers. It seamlessly integrates other critical building systems, creating a unified and intelligent operational environment. This holistic approach makes sure all the components work together to support the facility's primary mission: patient care.
These integrations almost always include:
CCTV and Security: Modern IP-based CCTV systems run over the network, providing high-definition monitoring for site security and patient safety. Designing them into the core network ensures reliable performance and makes future expansion easy.
Audio-Visual (AV) Systems: From multimedia systems in training rooms to digital signage in waiting areas, AV solutions rely on a stable network backbone to deliver information effectively.
Modern Telecoms (VoIP): Voice over IP (VoIP) phone systems are now the standard, offering far more flexibility than old-fashioned phone lines. But their reliability is entirely dependent on the quality of the network they run on.
By planning these systems as part of a single, cohesive design, you avoid the common pitfalls of siloed projects and create a more manageable, secure, and future-ready facility. For those tasked with this, our practical guide to designing the modern NHS network offers more detailed insights. This integrated strategy is the blueprint for an infrastructure that can not only handle today's demands but is also prepared for the future of digital health.
Implementing Unmanned Building Management Systems
When we talk about an ‘unmanned building’ in an NHS context, we’re not talking about ghost hospitals. In practice, it means creating intelligent, self-sufficient spaces that can operate securely with minimal or no permanent staff on-site. The goal is to build out fully autonomous unmanned building units that are efficient, secure, and can be managed from a central location. These systems are commonly used for satellite clinics, remote diagnostic centres, secure labs, or administrative outposts.
Getting this right isn’t just about installing some smart gadgets; it’s a complete shift in how we think about the design. Access control, power, and data can’t be treated as separate jobs. They must be engineered as one single, interdependent system from day one.
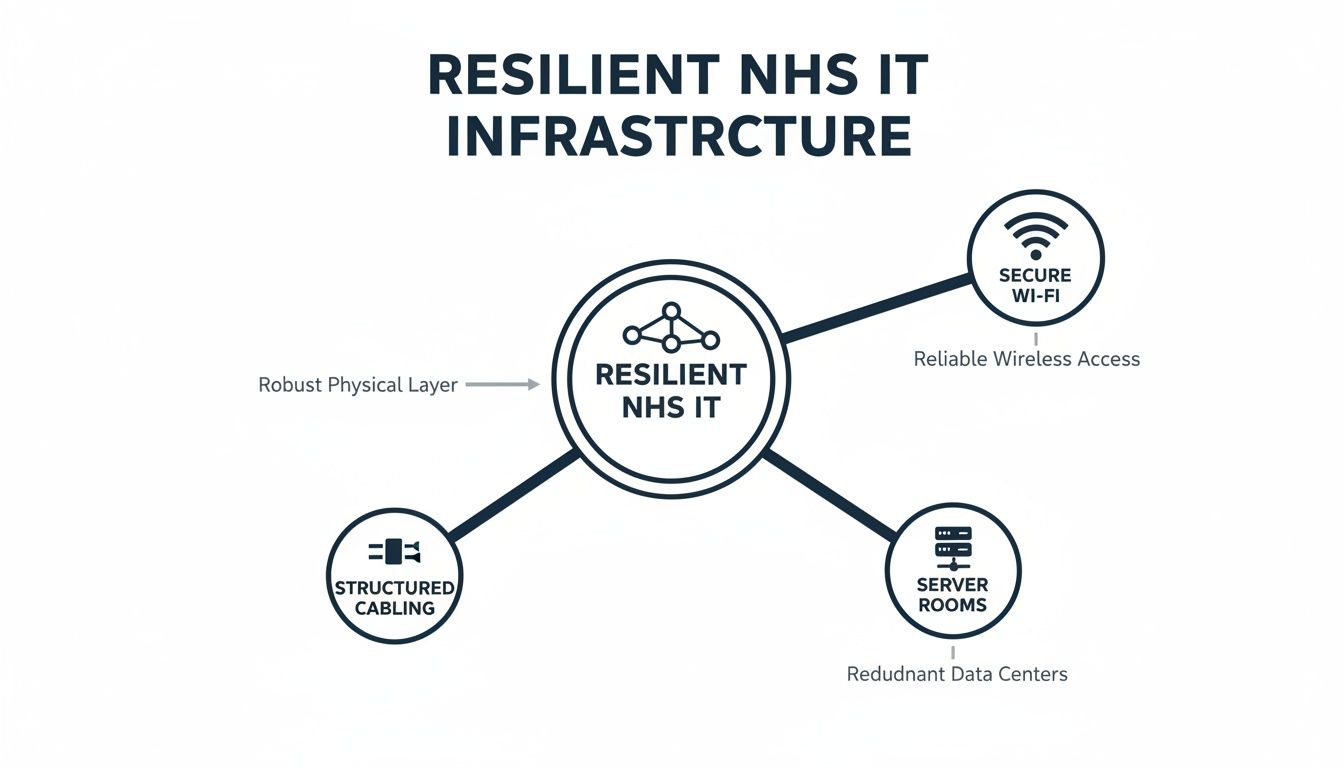
This is the bedrock of the entire concept. The diagram below shows how core IT systems like structured cabling, secure Wi-Fi, and server rooms form the resilient foundation needed for this kind of advanced facilities management.
Without that solid, integrated core, trying to build a reliable unmanned system on top is like building a house on sand. It simply won't work.
Why Many Unmanned Building Projects Fail
The single biggest reason these projects fail is a siloed design approach. When the teams planning access control, power, and data work in isolation, they inevitably miss the critical interdependencies. This leads to system conflicts, gaping security holes, and operational headaches down the line.
Imagine an access control system that goes down during a momentary power flicker because its electrical circuit wasn’t designed with the same resilience as the core network. The doors fail, security is compromised, and the integrity of the entire 'unmanned' facility is shattered.
This is why an integrated design is non-negotiable. Before you can even think about these advanced facilities, you need to understand how the underlying NHS network provides the foundation for autonomous buildings. It’s the critical first step.
How Access, Power and Data Must Be Designed Together
To build a reliable unmanned facility, these three pillars must be designed in lockstep from the very beginning. The network is the nervous system, the electrical installation is the lifeblood, and the access control system is the gatekeeper.
Data: The network must be flawlessly reliable. It's the communication backbone for everything—CCTV feeds, access logs, and remote management commands.
Power: Your commercial electrical installation and certification must be meticulous. We're talking dedicated circuits for security systems and UPS backups to guarantee continuous operation, even if the mains power goes out.
Access: The access control system has to integrate perfectly with the network for real-time monitoring while drawing its power from a resilient, backed-up source.
A successful unmanned facility is one where the data network knows the status of the door locks, the power system guarantees the network stays online, and the access system uses the network to report its status. They are three parts of one whole.
Real-World Reasons for Choosing Battery-less, NFC Proximity Locks
In these kinds of environments, traditional battery-powered locks are an operational nightmare. They create a constant maintenance cycle of checking and replacing batteries, introducing a recurring cost and a predictable point of failure.
This is where battery-less, NFC proximity locks are a complete game-changer for unmanned NHS facilities. These clever locks are powered directly by the NFC-enabled device—like a smartphone or an ID card—used to open them.
The real-world reasons for choosing them are compelling:
Zero Maintenance: With no batteries to replace, ever, the operational burden and associated costs are completely eliminated.
Full Audit Trail: Every single tap is logged digitally, creating a secure and auditable record of who entered and when, which is vital for compliance.
Enhanced Security: A building-wide power cut won't disable them, as they are powered by the user's credential, offering another vital layer of security.
Increased Reliability: By removing the most common point of failure (a dead battery), you create a far more dependable access control system.
Maintenance and Operational Considerations
While the aim is autonomy, these systems aren't "fit and forget." They still require a smart maintenance strategy. Remote monitoring is your best friend here, using integrated CCTV to visually verify the state of the facility and check for any physical problems without sending an engineer.
Your operational plan needs to include periodic physical checks of the hardware, scheduled software updates, and regular audits of the access logs to ensure security protocols are being followed. The goal is to shift from reactive, on-site fixes to proactive, remote management. That’s only possible when the core infrastructure is designed for resilience from the ground up.
By focusing on this integrated approach, facilities management NHS teams can confidently roll out secure, reliable, and truly autonomous units.
Executing a Seamless Project and Minimizing Downtime

When you’re running a project in a live clinical environment, there's only one objective that truly matters: zero disruption to patient care. This isn't something you can leave to chance. It demands a meticulously planned, phased approach that systematically takes the risk out of every stage, from the first site survey to the final handover.
The goal is simple. You want to move from a plan on paper to a functioning reality without any of the unwelcome surprises that could impact frontline services. Achieving that kind of seamless transition is the result of deep collaboration between your in-house teams and your specialist partner, orchestrating every step so that when the switch is flipped, everything just works.
The Phased Approach to Zero-Downtime Projects
The key to navigating the complexities of an NHS infrastructure project is a structured, phased methodology. For any facilities project where you need to minimise disruption, mastering the art of creating an effective project timeline is non-negotiable. This breaks down what can feel like a daunting task into a series of manageable, sequential stages, each with its own clear goals.
A typical project lifecycle will usually follow these core phases:
Site Surveys and Asset Audits: It all starts with a comprehensive audit of the existing environment. This means mapping out current infrastructure, identifying potential roadblocks, and building a detailed asset register to make sure the project scope is spot-on.
Collaborative Design and Planning: This is where your internal experts get in a room with external specialists. It's a critical phase that ensures the final design doesn't just work technically but also aligns perfectly with your operational needs and HTM compliance.
Installation and Certification: With the plan locked in, skilled engineers get to work, carrying out the installation to exacting standards. All work, from structured cabling to new power circuits, is then rigorously tested and certified to guarantee performance and safety.
Go-Live Support: The transition is never a solo flight. On-site engineers should be present during the crucial go-live period to provide immediate assistance, iron out any teething issues instantly, and give your clinical and IT staff complete peace of mind.
This phased approach is all about transforming a potentially high-risk, disruptive event into a controlled, predictable process. You're replacing uncertainty with a clear plan, ensuring the project delivers on its promises without ever compromising patient care.
The final piece of the puzzle is working with a specialist partner from day one. It helps de-risk the entire project, align the technical solution with your real-world operational goals, and build a clear roadmap for a successful outcome.
Your Questions, Answered
When it comes to the nuts and bolts of facilities management in the NHS, especially on modern infrastructure projects, a few key questions always pop up. Here are some straight answers based on what we see out in the field with estates and IT teams.
What Exactly is an Unmanned Building in the NHS?
In the NHS world, an unmanned building is a facility designed to run itself, without any permanent staff on-site. Think of a satellite clinic, a remote records office, or a secure pharmacy hub. The whole operation relies on a web of integrated technology for remote monitoring, access control, and security.
The idea is to create these fully autonomous units that are both incredibly secure and efficient. We achieve this by weaving together a rock-solid IT network with smart building systems, allowing everything to be managed from a central point and cutting the need for someone to be there 24/7.
Why Do These Unmanned Projects So Often Fail?
Honestly, most failures boil down to a siloed approach. When the access control guys, the power infrastructure team, and the data network specialists all design their bits separately, critical connections get missed. This is where you end up with gaping security holes, systems that fight each other, and an operation that's just fundamentally unstable.
For one of these facilities to be truly reliable, you have to plan the big three—access, power, and data—as a single, cohesive system right from the get-go.
A classic failure point we see is when a team specifies a highly resilient network but then plugs it into a standard electrical circuit with no UPS backup. One tiny power dip, and the entire security and access system can go dark, leaving the building completely vulnerable.
Why Are Battery-Less NFC Proximity Locks a Good Idea?
Battery-less, Near Field Communication (NFC) locks are a real game-changer for unmanned buildings. They're clever because they draw power directly from the user's NFC-enabled device—like an access card or a smartphone—the moment it makes contact. This completely does away with the need for any internal batteries.
This simple design choice has some huge real-world benefits:
Zero Maintenance: It completely wipes out the endless task (and cost) of checking and replacing batteries across dozens or hundreds of locks.
Massively Improved Reliability: With no batteries to fail, you eliminate a major weak link, ensuring the locks just keep working.
A Perfect Audit Trail: Every single time a door is opened, the event is logged digitally. This gives you a secure, undeniable record of who went where and when.
Planning a complex infrastructure project requires specialist expertise. Constructive-IT works with NHS trusts to design and deliver resilient, compliant, and future-proof facilities. To de-risk your next project and ensure a seamless execution, explore our services.






Comments