Facilities Manager NHS: A Practical Guide for the NHS - facilities manager nhs
- Craig Marston
- 4 days ago
- 17 min read
An NHS facilities manager is the person responsible for making sure hospitals and clinical spaces are safe, efficient, and up to scratch with all the rules. They’re the ones juggling everything from day-to-day maintenance and big infrastructure projects to strategic planning and new tech rollouts. It’s a role that directly impacts patient care and the smooth running of the entire Trust.
What used to be a purely operational job has become a seriously strategic one, demanding a sharp mix of technical skill and a clear vision for the future.
The Strategic Reality of Managing NHS Estates

Let’s be honest, the modern NHS facilities manager (FM) is much more than a building supervisor. You’re a strategic leader right at the heart of healthcare delivery. The real challenge is balancing the immense pressure of keeping everything running today with the forward-thinking needed to create resilient, patient-focused environments for tomorrow. It’s a constant battle between daily fire-fighting and long-term development.
This balancing act is made incredibly tough by the financial reality. Across the NHS, facilities managers are staring down a maintenance backlog that has ballooned to a staggering £11.6 billion. This figure really shines a light on the pressure cooker that is hard facilities management—a side of the industry that already makes up over 60% of the UK's entire FM market.
From Operational Tasks to Strategic Imperatives
The job description for a facilities manager nhs has stretched far beyond fixing leaks and managing the heating. Today, the role is packed with strategic duties that are absolutely critical for any modern healthcare Trust.
The big priorities on your plate now include:
Compliance and Governance: Making sure every inch of the estate meets the tough standards of things like the NHS Premises Assurance Model (PAM), which is vital for passing those all-important Care Quality Commission (CQC) inspections.
Technology Integration: Overseeing the rollout of complex IT infrastructure. We're talking about everything from the structured cabling that forms the digital backbone of the hospital to CCTV and access control systems that keep everyone safe.
Project and Procurement Management: Taking the lead on huge projects like new builds, ward relocations, or major system upgrades. This involves meticulous planning, choosing the right vendors, and keeping a firm grip on the budget.
Sustainability and Efficiency: Driving the push to meet Net Zero targets, slash operational costs, and make buildings more energy-efficient—all without ever compromising patient safety.
The core of the modern facilities manager's role is transformation. It's about evolving legacy infrastructure into a smart, resilient, and future-proofed estate that actively supports clinical excellence and enhances patient outcomes.
To really get a sense of the scope, it helps to break down how these duties connect to the bigger picture.
Key Responsibilities and Strategic Priorities for an NHS FM
This table summarises the core duties and the key strategic challenges that define the role of a facilities manager in the NHS today. It shows how the day-to-day tasks feed directly into the Trust's long-term goals.
Responsibility Area | Key Challenge | Strategic Goal |
|---|---|---|
Estate Compliance | Navigating complex and ever-changing regulations (PAM, CQC). | Achieve and maintain full compliance, ensuring a safe and legally sound environment. |
Infrastructure Management | Dealing with an ageing estate and a massive maintenance backlog. | Secure funding and implement upgrades to create a modern, reliable, and resilient estate. |
Technology & IT | Integrating new digital systems (EPR, IoT) into older buildings. | Build a robust digital infrastructure that supports modern clinical workflows and patient care. |
Project Leadership | Delivering large-scale projects on time and budget with minimal disruption. | Successfully manage capital projects that enhance capacity and improve the patient experience. |
Sustainability | Meeting ambitious Net Zero targets with limited capital investment. | Reduce carbon footprint and operational costs through energy efficiency and smart building tech. |
What this shows is that the role is no longer just about maintaining buildings; it's about steering the physical environment of the NHS toward a more efficient, sustainable, and patient-centric future.
Navigating the Daily Challenges
While high-level strategy is key, the day-to-day reality of managing a live hospital is relentless. As an FM, you have to guarantee that critical systems like HVAC, backup power generators, and medical gas pipelines have absolutely zero downtime. Any failure can have immediate and severe consequences for patients.
You also have the unenviable task of coordinating infrastructure works with the least possible disruption to active wards—a job that demands pinpoint scheduling and crystal-clear communication with clinical staff. To get a better handle on this, have a look at our guide to modernising and future-proofing NHS facilities.
Ultimately, it’s this ability to seamlessly merge top-level strategic vision with boots-on-the-ground operational excellence that defines a successful facilities manager in the NHS today.
Getting to Grips with NHS Compliance and Infrastructure Standards

For the facilities manager NHS trusts depend on, compliance isn’t just about ticking boxes. It’s the very bedrock of patient safety and a smoothly running hospital. Your world is a complex web of standards governing every nut, bolt, and cable in the healthcare estate, from the electrical wiring in a ward to the fire doors in a corridor.
This regulatory landscape is always shifting, which means you have to stay one step ahead. The goal is to build and maintain an estate where compliance is baked in from the start, not bolted on as an afterthought. Every new build, relocation, and system upgrade has to be right, first time.
The Role of the NHS Premises Assurance Model
At the heart of modern estate management sits the NHS Premises Assurance Model (PAM). Don't think of PAM as just another checklist. It's a proper framework for self-assessment that forces Trusts to take a hard, honest look at how they manage their buildings.
PAM has a real-world impact on everything you do. It shapes governance, risk management, and strategic planning. By demanding a tough, evidence-based approach, it influences maintenance schedules and long-term investment decisions, pushing for a more resilient and accountable estate.
The NHS Premises Assurance Model is designed to shift the focus from merely 'managing' facilities to actively 'assuring' their safety and fitness for purpose. It is the mechanism that connects day-to-day operational tasks with the highest levels of organisational governance and patient safety.
This framework is also becoming tightly linked to sustainability. As the NHS pushes towards its ambitious Net Zero targets, PAM is a key tool for making sure energy efficiency and environmental impact are built into all infrastructure planning and upgrade projects.
CQC Inspections and Why Meticulous Records Matter
While PAM sets the internal standard, the Care Quality Commission (CQC) is the external validator. When CQC inspectors walk through the door, they have one job: to make sure the environment is safe, effective, and well-led. For a facilities manager, this means your paperwork has to be flawless.
Your ability to instantly pull up clear, organised, and current records for fire alarm tests, electrical safety certificates, and everything in between can be the difference between a glowing report and a serious compliance warning. Gaps or messy records are a massive red flag for inspectors, often hinting at bigger problems in how the estate is run.
To fully grasp the complexities of safety and compliance, a guide to fire rated door safety, compliance, and liability is essential for facility and property managers within the NHS.
This is where modern Computer-Aided Facility Management (CAFM) systems have become indispensable. They take record-keeping from a headache-inducing pile of paper to a streamlined digital process, giving you a clear audit trail for every single compliance check and maintenance job.
Financial Realities and the Pressure to Comply
All this work happens against a tough financial backdrop. Healthcare facilities management in the NHS is a huge market, worth an estimated £6 to £8 billion a year. This is driven by old PFI contracts coming to an end, a staggering £13.8 billion maintenance backlog, and the government's New Hospital Programme.
This puts immense pressure on the facilities manager NHS teams to deliver modern, compliant hospitals on tight budgets. It’s no longer just about fixing what’s broken; it’s about making smart, strategic investments in infrastructure that’s resilient enough for the future. Every pound has to deliver maximum value for patient safety and long-term operational integrity.
Mastering IT Infrastructure in a Live Hospital Environment

A modern hospital doesn't just run on medicine; it runs on data. For the facilities manager NHS trusts rely on, getting to grips with IT infrastructure is no longer a niche skill—it’s now absolutely central to clinical care. This digital backbone supports everything from electronic patient records and diagnostic imaging to the life-sustaining medical devices on the wards.
Think of this network as the unsung hero of the healthcare environment. When it works flawlessly, clinical teams can deliver exceptional care without a second thought. But if it falters, the impact on patient safety and operational efficiency can be immediate and severe.
The Foundation of Digital Healthcare
At the heart of any hospital's digital operations is its physical network infrastructure. This isn’t just about plugging in a few computers. It's about engineering a resilient, high-speed ecosystem designed for the unique and relentless demands of a 24/7 clinical setting.
The key components of this foundation include:
Warrantied Structured Cabling: High-performance Cat6 and Fibre Optic cabling form the data superhighways. A 25-year warranty isn't just a guarantee; it's an assurance of long-term reliability and performance, crucial for avoiding disruptive and costly future repairs.
Secure Server Rooms: These are the heart of a hospital's data operations. They demand robust physical security, redundant power supplies, and precise climate control to protect the systems storing and processing sensitive patient information.
Resilient Wi-Fi Networks: From clinicians' tablets to IoT medical devices, reliable wireless connectivity is completely non-negotiable. A robust Wi-Fi network ensures seamless communication and data access across the entire estate.
It helps to think of this infrastructure like a hospital's circulatory system. The server room is the heart, the structured cabling is the network of arteries and veins, and the data itself is the lifeblood. A blockage or failure anywhere in that system can have critical consequences.
The Zero Disruption Challenge in Live Wards
One of the greatest challenges for any facilities manager NHS professionals face is overseeing infrastructure upgrades in a live hospital. Unlike a corporate office, you can't simply shut down a ward for a day to run new cables. The work must be done with surgical precision to ensure zero disruption to patient care.
This means installations often happen out of hours, following strict infection control protocols to contain dust and debris. It requires meticulous planning and constant communication between the facilities team, IT specialists, and clinical staff to navigate active environments without getting in the way of ongoing medical procedures.
The ultimate measure of success for an infrastructure project in a live hospital is invisibility. The goal is to complete a complex technical upgrade so seamlessly that clinical staff and patients are entirely unaware it even happened.
This challenge is amplified by the sheer scale and complexity of modern healthcare IT. Recent trends show a move towards large-scale partnerships to manage these projects. For instance, Siemens secured a landmark £1 billion contract to provide total facilities management for multiple NHS hospitals, emphasising digital solutions for infrastructure. This reflects a broader shift where facilities teams collaborate with specialists for critical tasks like cabling and server room expansions to minimise downtime during upgrades.
Integrating Electrical, CCTV and Data
A truly successful facilities strategy recognises that IT infrastructure doesn't exist in a vacuum. Key systems must be designed and installed as part of a unified whole, not as separate, siloed projects.
Commercial Electrical Installation: Your data network is only as reliable as its power source. Professional commercial electrical installation and certification are vital, ensuring that server rooms have clean, uninterruptible power and that data points are safely and correctly energised.
Integrated CCTV: Modern security cameras are network devices. Integrating their installation with your main cabling project is more efficient, reduces costs, and ensures your security system has the robust connectivity it needs to function correctly.
Planning these elements together avoids the common pitfall of having to retrofit systems, which is always more disruptive and expensive. When decommissioning old IT equipment, facilities managers must also prioritise data security, often by securing a certificate of destruction for hard drives to ensure full compliance and protect patient data.
For more detailed strategies on building a cohesive digital backbone, check out our article on designing the modern NHS network.
What Does an ‘Unmanned Building’ Really Mean for the NHS?
The idea of an ‘unmanned building’ might sound a bit futuristic, but for spaces like out-of-hours clinics, secure admin blocks, or remote storage facilities, it’s an incredibly practical solution. In simple terms, it means creating a self-sufficient unit that can be accessed, monitored, and managed from a distance, without needing staff permanently on-site.
This isn’t about replacing people; it’s about deploying your resources more intelligently. An unmanned building gives authorised personnel—whether it's a clinician, a maintenance engineer, or a records clerk—secure access whenever they need it. Meanwhile, the facilities manager NHS teams rely on can keep a watchful eye over everything from a central hub.
Why So Many Unmanned Building Projects Go Wrong
The classic mistake is treating an unmanned building project like a shopping list of separate jobs. You get the security team to handle access control, the IT team to manage data, and the estates team to look after the power. This siloed approach is a recipe for failure.
When these critical systems are designed in isolation, they can't talk to each other. The access control system might not be able to flag a power cut to the central office, or the CCTV system could lose its connection, leaving the entire building vulnerable. A truly autonomous building needs a unified design right from the start.
The success of an unmanned building hinges on a simple principle: access, power, and data are not separate systems but three legs of the same stool. If one is weak or disconnected from the others, the entire structure collapses.
This integrated approach makes sure every component works in harmony, creating a resilient and genuinely autonomous unit you can trust to function without someone constantly watching over it.
Designing Access, Power, and Data as a Single System
To build a truly autonomous unit, these three elements have to be woven together from the first planning meeting. It’s about creating a single, cohesive ecosystem where each part supports the others, guaranteeing reliability and security around the clock.
Here’s how they need to work in unison:
Access Control: The system shouldn’t just open doors. It must log every single event and report its own health status back to your central hub, and for that, it needs a rock-solid data connection.
Power Supply: Uninterruptible Power Supplies (UPS) are non-negotiable. They must be powerful enough to keep not just the locks running, but also the CCTV, network switches, and any environmental sensors, even during a mains outage.
Data Connectivity: A reliable network connection is the building's central nervous system. It’s what carries access logs, CCTV footage, and system health alerts, making genuine remote management possible.
By planning the commercial electrical installation and certification at the same time as the network cabling and security hardware, you create a seamless infrastructure where power and data are delivered exactly where they need to be, with redundancy built in from day one.
The Case for Battery-Less NFC Proximity Locks
For any NHS facilities manager, maintenance is a constant headache. This is exactly why battery-less, Near Field Communication (NFC) proximity locks are such a game-changer for unmanned buildings. Traditional battery-powered locks create a huge operational burden—they need regular checks and replacements, and a dead battery means a lockout.
The real-world reasons for choosing this technology are compelling:
Zero Maintenance: With no batteries to change, these locks remove a major point of failure and a recurring maintenance task. This slashes the total cost of ownership.
High Reliability: The lock gets its power from the user's NFC-enabled device (like a keycard or smartphone) at the moment of entry. This makes the system incredibly dependable.
Enhanced Security: NFC uses secure, encrypted communication, making it far harder to clone or intercept than older magnetic stripe or basic RFID systems.
These locks are perfect for secure drug storage rooms, IT server closets, and remote clinics where sending an engineer just to replace a battery is impractical and expensive. Their built-in reliability is what makes it possible to create fully autonomous units that need minimal human intervention.
Operational and Maintenance Planning
Even though battery-less locks cut down on maintenance, the overall system still needs a clear operational plan. This should include scheduling regular checks for the UPS batteries that power the network and CCTV systems, as well as testing the remote data link to ensure it remains stable and responsive.
Partnering with a specialist who understands how to integrate these systems from the ground up de-risks the entire project. This ensures your unmanned facilities are not just technologically advanced, but also operationally sound and secure for the long haul.
Your Project Checklist for NHS Infrastructure Upgrades
Overseeing a major infrastructure project in an NHS setting is a high-stakes balancing act. As the facilities manager NHS trusts rely on, you're tasked with delivering upgrades that are on time, on budget, and — most importantly — have zero impact on patient care. A pragmatic, well-structured checklist isn't just helpful; it's your most powerful tool for cutting through the complexity.
Thinking about the project chronologically, from the first spark of an idea to the final switch-on, is the best way to keep things manageable. This approach breaks down a daunting undertaking into a clear series of achievable steps, making sure no critical detail falls through the cracks. It's about moving from reactive fire-fighting to proactive project leadership.
Initial Planning And Stakeholder Engagement
Before a single cable gets ordered or a contractor is called, the real work begins. This foundational stage is all about deep discovery and getting everyone on the same page. The first step is always a comprehensive site survey — and I don't mean a quick walk-through. This needs to be a detailed analysis of the existing infrastructure, potential roadblocks, and the physical constraints of the building.
Next, you have to nail down the technical specifications. Vague requirements are the root cause of scope creep and blown budgets. Your specs need to be precise enough to form the basis of a watertight tender document, leaving absolutely no room for misinterpretation.
Crucially, this is the time to get your key stakeholders in a room. Bring the clinical leads, IT teams, and estates personnel into the conversation right from the start. Their input is gold; it helps you understand the real-world operational workflows and ensures the final solution actually works for the people using it day in, day out.
Vendor Selection And Due Diligence
Choosing the right partner is arguably the most important decision you'll make. Your selection criteria must go far beyond just picking the most attractive price. An infrastructure partner without a deep, practical understanding of the unique NHS environment can quickly become a serious liability.
Look for vendors who can prove their worth with:
Proven NHS Experience: They should have a portfolio of successful projects carried out inside live hospital environments.
Relevant Certifications: This covers everything from electrical safety (NICEIC) to data cabling warranties from recognised manufacturers.
Infection Control Understanding: A partner must have robust, documented protocols for working in clinical areas to prevent dust and debris contamination.
When you're evaluating potential partners, focus on their process as much as their price. A vendor who asks you detailed questions about clinical operations and your infection control policies is a vendor who truly understands the unique demands of the NHS.
The process flow below shows how critical it is to design access, power, and data systems as a single, unified whole, especially for robust unmanned or automated building systems.
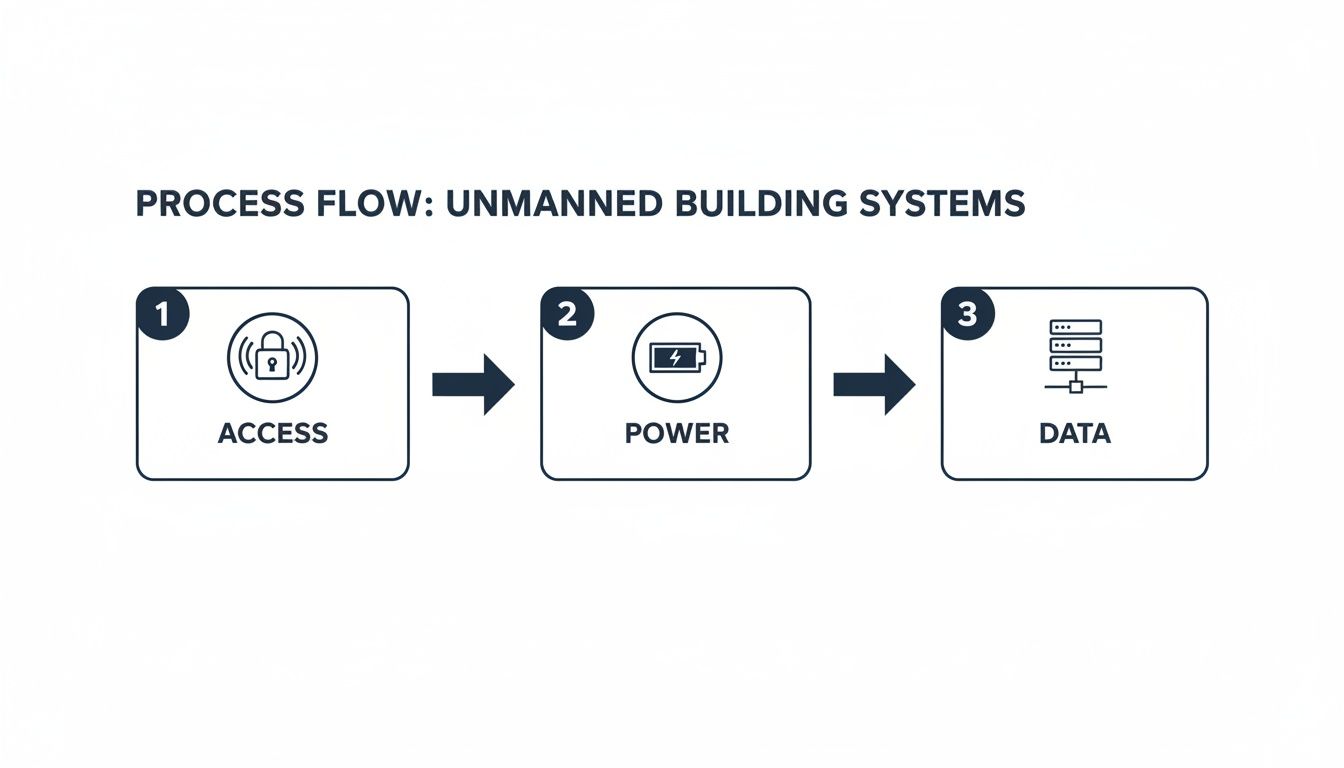
This kind of integrated thinking is key. A project's success hinges on weaving these core components together right from the very beginning of the planning phase.
Choosing the right partner is about balancing essential qualifications with value-added expertise. This table breaks down what to look for when vetting potential vendors for your project.
Vendor Selection Criteria for Critical NHS Infrastructure Projects
Criteria | Essential (Non-Negotiable) | Desirable (Added Value) |
|---|---|---|
Experience | Demonstrable track record of successful projects in live NHS environments. | Case studies showing projects of similar scale and complexity to yours. |
Compliance | Full adherence to HTM/HBN standards and infection control protocols. | Proactive suggestions for improving compliance or operational efficiency. |
Certifications | NICEIC electrical accreditation; Manufacturer-backed cabling certifications. | Accreditations in related fields like network security or building management systems. |
Project Management | Clear communication processes and a dedicated, named project manager. | Experience using collaborative project management software for real-time updates. |
On-Site Conduct | Strict policies on staff conduct, cleanliness, and minimising disruption. | Staff trained specifically for working in sensitive clinical environments. |
Support | A clear plan for on-site engineering support during the go-live phase. | Offers extended post-project support and comprehensive staff training. |
Ultimately, a partner who ticks all the "Essential" boxes is qualified. A partner who also brings the "Desirable" attributes to the table is one who will actively de-risk your project and become a genuine asset to your team.
Execution And Go-Live
With a trusted partner selected, the focus shifts to getting the job done. This phase demands meticulous project management and crystal-clear communication. Regular progress meetings with your vendor and internal stakeholders are non-negotiable to keep everyone in the loop and tackle any issues the moment they appear.
The final, and most critical, step is the on-site go-live. A quality partner doesn't just hand over the keys and walk away. They will provide hands-on engineering support during the entire transition to guarantee a smooth switchover, troubleshoot any immediate teething problems, and ensure your own team is confident with the new system. This direct, on-site support is what truly de-risks a project and ensures a successful outcome.
Ensuring Project Success from Procurement to Go-Live
Turning strategic insight into a successful, real-world project is the ultimate measure of a facilities manager's effectiveness. That journey, from the initial procurement decision to a fully operational, ‘go-live’ system, is often fraught with potential pitfalls. True success hinges on integrated planning, selecting the right specialist partners, and keeping a laser focus on the long-term value your project delivers.
This final stage isn’t just about finishing a job; it’s about future-proofing the estate. Choosing a partner who provides warrantied solutions isn't just a bonus—it's a critical assurance of quality and long-term reliability. A 25-year manufacturer-backed warranty on structured cabling, for instance, completely de-risks your investment and guarantees that the infrastructure will support clinical needs for decades to come.
The Value of a Collaborative Partnership
The old-school client-vendor relationship is outdated for complex NHS projects. What you really need is a genuinely collaborative partner who functions as an extension of your own team. They should be just as invested in your project's success as you are, offering proactive advice and working shoulder-to-shoulder with you to overcome challenges as they arise.
This collaborative spirit is most crucial during those final stages. A partner who provides dedicated, on-site go-live support shows a commitment that goes far beyond simply completing an installation. Having their engineers present during the switchover is invaluable for troubleshooting, ensuring a seamless transition, and giving your internal teams the confidence to take ownership of the new systems.
Choosing a partner is about more than technical skill; it's about finding an ally who understands the stakes. Their ability to de-risk your project through meticulous planning, proven NHS experience, and hands-on support is the single greatest factor in achieving a successful outcome.
This approach ensures that every project, whether it's a new build or a critical upgrade, delivers a resilient, compliant, and highly effective environment. It’s this strategic mindset that allows a facilities manager NHS teams depend on to support clinical excellence for years to come. By moving beyond a simple procurement checklist to a holistic partnership model, you build a foundation for lasting success.
From Blueprint to Lasting Legacy
Ultimately, every infrastructure project is about more than just technology. It’s about creating physical spaces that enable the highest standards of patient care. Your role is to ensure that the initial blueprint translates into a lasting legacy of safety, efficiency, and resilience. For a deeper dive into the specific strategies that can help you achieve this, consider exploring our guide on mastering IT infrastructure project management.
By prioritising integrated planning, demanding warrantied solutions, and insisting on a collaborative partnership, you can confidently deliver projects that not only meet today's needs but also anticipate tomorrow's challenges.
Your Questions Answered: An NHS Facilities Manager's FAQ
We get a lot of questions from facilities managers on the ground in the NHS. Here are straight answers to some of the most common ones we hear.
What’s the Biggest Hurdle When Upgrading IT Cabling in a Live Hospital?
Without a doubt, it's managing the project without disrupting clinical services or compromising patient safety. It’s one thing to run cables in an empty office block; it’s another thing entirely when you’re working around live wards, operating theatres, and sensitive equipment.
This is where meticulous planning is non-negotiable. You’re dealing with strict infection control protocols like dust containment, and all work has to be scheduled around the hospital’s rhythm, often during nights or weekends. A specialist partner with proven NHS experience is crucial. They’ll know how to phase the project to keep critical systems online throughout, making the whole process feel seamless for staff and patients.
How Does the NHS Premises Assurance Model (PAM) Affect Who I Can Hire?
The NHS Premises Assurance Model (PAM) is all about governance and managing risk across the entire estate. It means you can't just hire any contractor; you need a partner whose work is fully documented and compliant. When selecting vendors, you have to be confident they can provide comprehensive paperwork and certifications for everything they install.
This is where warrantied solutions and detailed post-installation reports are vital. This evidence-based approach is exactly what you need to meet PAM’s stringent assurance requirements and prepare for any CQC inspections.
A key responsibility for any facilities manager NHS trusts employ is ensuring every vendor can demonstrate clear compliance. Their ability to provide thorough documentation is a direct reflection of their suitability for healthcare projects.
Why Should I Bundle CCTV, Access Control, and IT Infrastructure Projects Together?
Integrating these systems right from the start is simply smarter, more cost-effective, and builds a far more resilient facility. When you design them as one unified system, you ensure that power, data, and access control work together flawlessly—a core requirement for any modern, securely managed building.
Taking this approach saves you from the headache and expense of retrofitting later on. It also streamlines the project itself, as you’re managing fewer vendors on-site. The end result is a cohesive system where every component, from the CCTV cameras to the structured cabling, is designed to work in harmony from day one.
Planning a critical infrastructure project requires a partner who understands what’s at stake. Constructive-IT delivers warrantied, compliant, and seamlessly integrated solutions for the NHS—from structured cabling to complete server room builds—ensuring your project succeeds with zero disruption.
Discover how we can support your next project at https://www.constructive-it.co.uk.






Comments