NHS Facilities Manager: A Complete Guide for nhs facilities manager
- Craig Marston
- 3 days ago
- 20 min read
Being an NHS facilities manager means you’re on the front line of keeping healthcare estates running. Your job is to make sure every building and all its services are safe, compliant, and efficient enough to support first-class patient care. But the role has exploded beyond traditional maintenance. Now, it's about strategic tech planning, tackling a monumental infrastructure backlog, and hitting critical net-zero targets. You are absolutely central to the operational resilience of the UK's healthcare system.
The Evolving Role of the NHS Facilities Manager

Managing an NHS estate isn’t just about keeping the lights on anymore. As an NHS facilities manager, you’re performing a complex balancing act, juggling immense pressures with massive strategic responsibilities. One minute you’re dealing with ageing infrastructure, the next you're planning for the digital future of healthcare.
This guide isn’t about routine maintenance. It’s a practical roadmap for planning and delivering the kind of complex IT projects that have become business-as-usual—from new builds and relocations to essential Wi-Fi upgrades. We’ll offer real-world, actionable advice designed for the unique, high-stakes NHS environment.
Navigating Unprecedented Challenges
The scale of the challenge you're up against is staggering. Across the NHS, facilities managers are grappling with a maintenance backlog that has now hit £11.6 billion. This isn't just an abstract number; it has a direct impact on patient care, causing around 5,400 clinical service incidents every single year due to estates and facilities failures. It’s a stark reminder of the human cost of deferred maintenance.
The modern NHS facilities manager is a strategist, a technologist, and a guardian of patient safety. The focus has shifted from reactive repairs to proactive, technology-driven estate management that directly enables better clinical outcomes.
This new reality demands a forward-thinking approach. Your core responsibilities have expanded to include:
Future-Proofing Infrastructure: Making sure both new and existing buildings can support the next generation of medical tech, from digital patient records to the Internet of Things (IoT).
Ensuring Digital Compliance: Sticking to rigorous NHS digital security standards and data protection regulations in every single infrastructure project.
Meeting Sustainability Goals: Aligning all estate management work with the NHS’s firm commitment to achieving Net Zero carbon emissions.
A key and growing part of the job is implementing robust strategies for preventing healthcare associated infections, an area where building design, ventilation, and maintenance play a absolutely crucial role.
The IT and network infrastructure you manage is the backbone of modern clinical care. Here’s a look at some common projects and how they directly translate into better services for patients and staff.
Key IT Infrastructure Projects and Their Clinical Impact
Project Type | Core Objective | Impact on Clinical Services |
|---|---|---|
New Ward/Building IT Fit-Out | To equip a new clinical space with a fully functional, reliable network from day one. | Enables immediate use of Electronic Patient Records (EPR), diagnostic imaging, and communication systems, ensuring seamless patient care continuity. |
Wi-Fi Network Upgrade | To provide fast, secure, and ubiquitous wireless connectivity across the entire estate. | Supports mobile workstations (WoWs), allows clinicians to access patient data at the bedside, and improves patient experience through visitor access. |
Structured Cabling Refresh | To replace outdated copper or fibre cabling with modern, high-bandwidth infrastructure. | Increases network speed and reliability for data-heavy applications like PACS imaging and telemedicine, reducing delays in diagnosis and treatment. |
Server Room/Comms Room Expansion | To increase the capacity and resilience of the core network hardware environment. | Enhances the performance of all connected clinical systems, reduces the risk of system-wide outages, and supports the growth of digital services. |
These projects are fundamental, not just for operational efficiency but for elevating the standard of care across the board.
Why a Specialist Partner is Crucial
The sheer complexity of these projects—blending electrical, network, and security requirements, often within live clinical settings—calls for specialist expertise. Trying to manage these intricate upgrades in-house can stretch your resources thin, introduce unacceptable risks, and pull your focus away from core operational duties.
A specialist partner with proven NHS experience brings the deep technical knowledge and project management discipline needed to get the job done on time, on budget, and without disrupting patient services. Our guide offers more insights into modernising and future-proofing NHS facilities, showing how a collaborative approach is the key to success.
Strategic Project Planning and Stakeholder Alignment
Successful NHS infrastructure projects are never just about the tech. They’re built on a rock-solid understanding of clinical workflows. As an NHS facilities manager, your first job is to look past the blueprints and cable diagrams and see the project through the eyes of the clinicians and patients who will rely on it every single day. Frankly, this is where projects either fly or fail.
It all kicks off with proper site surveys and asset audits. This isn’t just a box-ticking exercise of counting data ports or measuring comms rooms. It's about mapping the complex web of dependencies that ties your clinical, IT, and operational teams together. How does a ward manager use the network for patient observations? Which specific medical devices need flawless connectivity during a ward move? Answering these questions is how you turn urgent clinical needs into a technical brief that actually makes sense.
Assembling Your Multi-Disciplinary Project Team
No NHS project has ever succeeded in a silo. Your role is to bring together and lead a multi-disciplinary team that represents every corner of the hospital's operations. Get this right, and you’ll sidestep costly mistakes and operational headaches later on.
Your core project team absolutely must include:
Clinicians: Your nurses, doctors, and ward managers. They bring the real-world perspective on daily workflows, peak times, and the potential impact of any disruption. Their insight is gold.
IT Specialists: The in-house IT team knows the existing network architecture, security protocols, and integration challenges inside out. They are your technical lifeline.
Estates Staff: This group understands the building’s physical quirks and limitations—everything from power constraints to the asbestos register and fire compartmentation.
Infection Control Practitioners: For any work in a live clinical environment, their input isn't just important; it's non-negotiable. Patient safety is always the top priority.
By getting these people talking from day one, you build a shared understanding and a collective sense of ownership. This alignment is what ensures you deliver a project that genuinely helps patient care, rather than getting in the way.
Translating Clinical Needs into a Technical Brief
With your team in place, the next challenge is creating a technical brief that an external partner can execute with pinpoint accuracy. This document is the project’s constitution. It defines what success looks like and guarantees the outcome is all about patient safety and quality of care. A proper brief goes way beyond just asking for "Cat6 cabling."
It should detail performance requirements that are tied directly to clinical scenarios. For instance, instead of just saying you need Wi-Fi, specify the need to support 30 wireless medical devices per bay with zero packet loss and seamless roaming for staff carrying voice-over-IP handsets. That level of detail kills ambiguity and makes your delivery partner accountable for a solution that works in the real world, not just on paper.
An effective technical brief is a story about how technology will enable better patient care. It connects every cable, switch, and access point back to a specific clinical function, ensuring the final solution is fit for its critical purpose.
Modern project planning for NHS facilities also means looking at sustainable electrical infrastructure solutions. Balancing operational performance with environmental impact is becoming a massive part of long-term estate strategy and hitting those vital Net Zero targets.
This kind of meticulous planning is also being driven by new governance frameworks. NHS facilities managers are on the frontline of a £27 billion public sector facilities management spend. The revised NHS Premises Assurance Model (PAM) puts a much bigger emphasis on evidence-based reporting and prioritising investment in high-risk buildings to tighten up safety and governance. You can get more detail on these new requirements and what they mean for estates management in this overview of the revised NHS Premises Assurance Model on YouTube.
Ultimately, your role in this phase is one of translation—turning the language of clinical needs into the precise language of technical delivery. This foundational work ensures the infrastructure you build is not just compliant and robust, but a true enabler of world-class healthcare.
Developing Technical Specifications and Compliant Procurement
With a solid plan in place and your stakeholders on the same page, it's time to get into the nitty-gritty—the technical details that form the bedrock of the entire project. As an NHS facilities manager, this is where your ability to define precise, future-proof specifications for critical infrastructure really comes into play. You’re translating the needs of clinicians and department heads into a clear, actionable blueprint for your external partners.
This means defining the requirements for everything from structured cabling (Cat6/Fibre) to the Local Area Network (LAN), Wide Area Network (WAN), and the high-density Wi-Fi that keeps a modern hospital running. It’s not just about what you need today; it’s about anticipating the demands of tomorrow. In a healthcare environment where new medical technologies constantly raise the performance bar, future-proofing isn’t just a buzzword—it's non-negotiable.
Crafting Robust Technical Specifications
A vague specification is an open invitation for ambiguity, risk, and misaligned quotes. To attract the right level of expertise and guarantee a successful outcome, your technical brief has to be meticulously detailed. It needs to account for scalability, iron-clad security, and the unique physical constraints of a hospital setting.
Your specifications should always address these core areas:
Structured Cabling (Cat6/Cat6a/Fibre): Pinpoint the exact standard of cabling needed to handle your current and future bandwidth demands. Define containment routes, detail fire-stopping requirements, and—crucially—demand a manufacturer-backed 25-year warranty. This guarantees long-term performance and protects your investment. For a deeper look into the nuances, you can explore our essential guide to data cabling installation.
High-Density Wi-Fi: Don't just ask for Wi-Fi; define performance metrics based on real-world clinical scenarios. Specify the capacity needed to support a high concentration of medical devices, staff communication tools, and patient services, all without a hint of performance lag. This includes planning for seamless roaming as staff move between access points.
LAN/WAN Architecture: Get specific about your network switches, routers, and firewalls. This includes detailing Power over Ethernet (PoE) budgets for devices like IP phones and CCTV cameras, and outlining your network segmentation (VLAN) strategy to tighten security and manage traffic effectively.
NHS Digital Security Standards: Make adherence to NHS cybersecurity protocols a mandatory requirement from the very start. Your spec must insist that any proposed solution complies with all relevant standards to protect sensitive patient data and keep your network resilient against threats.
A strong technical specification leaves no room for interpretation. It ensures every tender response is based on the same clear, high standards, allowing you to compare potential partners on a true like-for-like basis.
Navigating Compliant Procurement Frameworks
Procuring services within the NHS means sticking to strict, transparent processes designed to ensure value for money and fair competition. Frankly, the most efficient and compliant route is often through established procurement frameworks that give you access to qualified, pre-vetted partners.
One of the key players here is the Crown Commercial Service (CCS). These frameworks do the heavy lifting for you by providing a list of suppliers who have already been assessed for their financial stability, technical skill, and compliance with public sector rules.
For IT infrastructure projects, a framework like RM6232 (Vertical Application Solutions) is a great place to start, as it covers a huge range of technology solutions and services. Using these frameworks saves a massive amount of time and administrative headache, giving you confidence that any supplier you engage has already met a baseline standard of quality.
Attracting the Right Expertise Through Your Tender
Once your specs are locked down and you’ve picked a procurement route, the next job is to create a tender document that attracts partners with the right blend of technical skill and genuine healthcare experience. Just asking for a price won't cut it. You need to dig into a supplier’s methodology, their track record, and their understanding of the live NHS environment.
Your tender evaluation criteria should heavily weight the following:
Proven NHS Experience: Ask for specific case studies of projects they’ve delivered within live hospital environments.
Cybersecurity Credentials: Request proof of certifications like Cyber Essentials Plus, which demonstrates a serious commitment to security.
Staged Migration Planning: Require bidders to outline exactly how they’ll minimise clinical disruption during the rollout.
Dedicated Go-Live Support: Make sure the tender specifies on-site engineering support during that critical transition phase.
By focusing your tender on these areas, you shift the conversation from cost to value. You’ll attract partners who get that a successful NHS project isn't just measured by its technical brilliance, but by its ability to enhance patient care without causing chaos. This rigorous approach ensures you select a partner truly capable of delivering a resilient, secure, and future-ready infrastructure solution.
Managing Implementation with Minimal Clinical Disruption
This is where the rubber meets the road. Even the most perfectly planned NHS infrastructure project can fall apart during execution. In a live hospital, the stakes are sky-high; every single action has to be weighed against its potential impact on patient care. As an NHS facilities manager, your job now is to become the guardian of clinical continuity.
It’s a real shift in mindset. You're moving from being a pure project manager to a clinical liaison. The challenge isn't just about rolling out new tech—it's about doing it in a dynamic, high-pressure world where patient safety is the only thing that truly matters. This means scheduling work around clinical rotas, sticking to uncompromising infection control rules, and keeping an open line of communication with ward managers at all times.
Success comes down to one thing: a staged migration. A "big bang" approach, where you flip the switch on a whole new system at once, is far too risky for a hospital. A phased rollout—like a ward-by-ward cabling or Wi-Fi upgrade—lets you contain risks, troubleshoot unexpected issues, and apply lessons learned to the next stage.
Creating a Bulletproof Phased Migration Plan
During implementation, your migration plan is the single most important document you have. It’s the detailed script that coordinates your external partner, your in-house IT team, and the clinical staff on the ground. It needs to be a living document, shared and agreed upon by everyone involved.
Your plan absolutely must define:
Out-of-Hours Work Schedules: Get granular. Pinpoint the exact times for noisy or disruptive jobs, making sure they happen when clinical activity is at its lowest ebb. This almost always means night or weekend shifts.
Infection Control Procedures: Spell out the specific measures for dust suppression, waste removal, and tool management. Everything must be pre-approved by your infection control team.
Temporary Connectivity Solutions: If a ward’s network has to go down, how will staff access critical systems like the Electronic Patient Record (EPR)? Outline the plan for temporary wireless bridges or cellular hotspots.
Rollback Criteria: What’s the abort trigger? Establish clear, pre-defined conditions for halting a migration phase and reverting to the previous state if something goes wrong.
This level of detailed planning is more important than ever. A huge £1 billion contract recently awarded to Siemens by the NHS shows a major shift towards integrated, digital-first healthcare. With hospital bed occupancy rates sitting at an average of 72.0% over the last two years, our reliance on dependable IT has never been greater. It’s why managing these projects from end to end with minimal disruption is so vital. You can find more insights on the UK facility management market on Technavio.com.
Any technical upgrade has to follow a logical sequence, starting from the physical layer and working up.
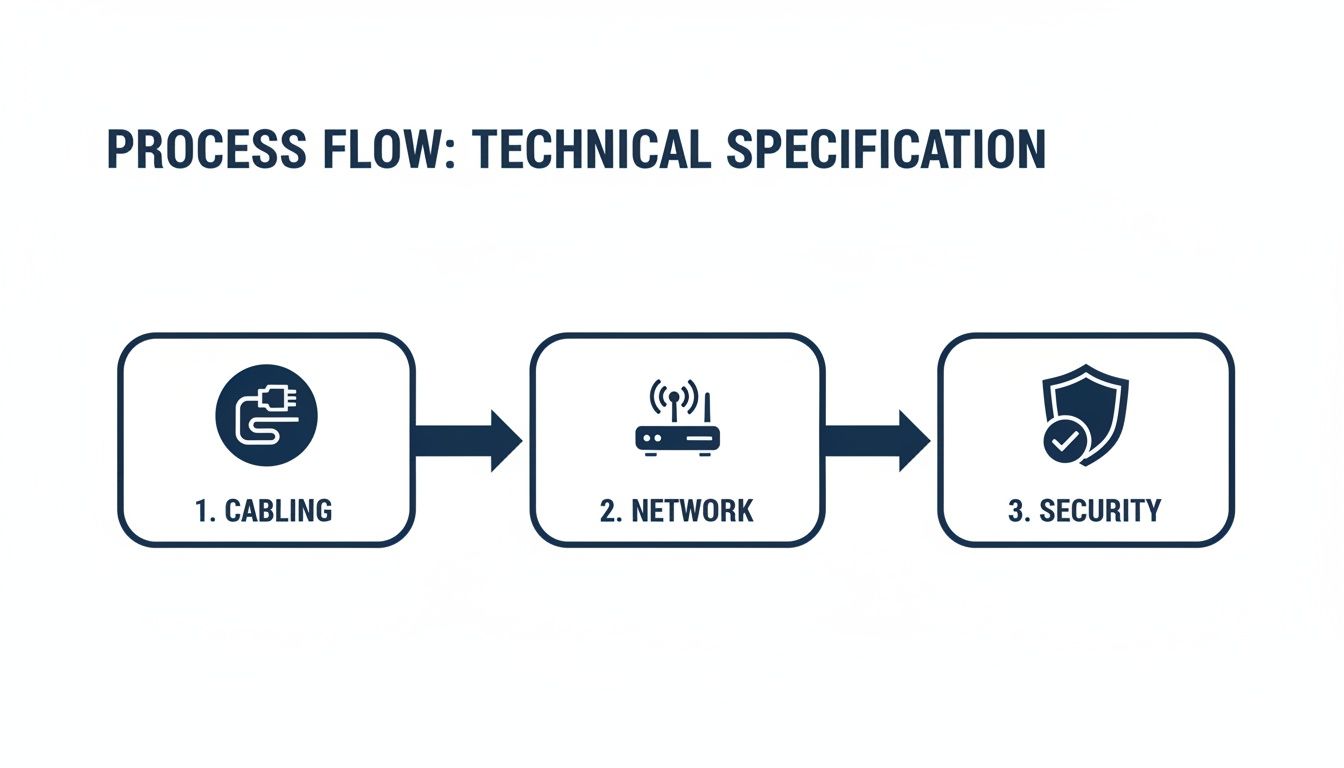
This flow shows how everything is built on a foundation. You start with the physical cabling, move to the network configuration, and finish with security. The key takeaway is that each stage depends on the one before it. A flaw in the cabling will ripple upwards, inevitably compromising network performance and security.
To illustrate how a staged migration works in practice, let's look at a common scenario: upgrading the Wi-Fi on a single ward. The goal is to avoid any interruption to clinical workflows.
Phased Migration Strategy for a Ward-Level Wi-Fi Upgrade
Phase | Key Actions | Stakeholder Communication | Contingency Plan |
|---|---|---|---|
Phase 1: Pre-Install (Out of Hours) | Install and cable new Access Points (APs) alongside existing ones. New APs remain offline. | Inform ward manager of overnight engineering presence. No disruption to users expected. | If installation runs over, secure all new equipment and cabling until next scheduled window. |
Phase 2: Configuration & Testing | IT and partner configure new APs remotely. A single test device (e.g., a spare WoW) is connected. | Update IT and ward manager that the new network is being tested but is not live for clinical use. | If test device fails to connect, troubleshoot remotely. No impact on the live clinical network. |
Phase 3: Staged Go-Live | During a planned quiet period, switch a small number of non-critical devices to the new network. Monitor performance. | On-site engineer liaises directly with nurses to manage the device switchover and gather immediate feedback. | If issues arise, immediately switch affected devices back to the old network. Old network remains fully active. |
Phase 4: Full Cutover & Decommission | Once stable, migrate all remaining devices to the new Wi-Fi. Old APs are switched off but left in place. Decommissioned after 48 hours. | Announce full migration is complete. Provide on-site engineer support for the first full day shift. | Keep old network ready for immediate rollback. If major issues occur, switch all devices back. |
This methodical approach allows you to control the variables, test at each stage, and ensure that by the time you make the final switch, you’ve ironed out any potential problems without ever putting patient care at risk.
The Critical Role of Go-Live Support
No matter how perfect your plan is, the moment of transition—the "go-live"—is always tense. This is why having dedicated, on-site support from your implementation partner isn't a luxury; it's an absolute necessity. Having their engineers physically present on the ward as the new system is turned on provides immediate troubleshooting and, just as importantly, reassurance for the clinical staff.
The real test of a project is not the handover, but the first Monday morning shift after go-live. On-site engineering support during this critical period is the best insurance against minor glitches escalating into major clinical incidents.
Picture this: a new Wi-Fi network goes live on a surgical ward. A nurse suddenly finds her mobile workstation (WoW) won't connect. With an engineer on-site, the issue—maybe a simple driver conflict—is diagnosed and fixed in minutes. Without that immediate presence, the problem becomes a helpdesk ticket, potentially leaving the ward without a critical tool for hours.
It's this rapid, hands-on response that protects clinical operations and builds confidence in the new technology. This is the standard of execution an experienced NHS facilities manager should always demand.
Integrating Systems for Unmanned Building Management

Real operational efficiency across the modern NHS estate often hinges on how well your systems talk to each other, especially in remote or supplementary buildings. As an NHS facilities manager, you might find yourself responsible for unmanned units—think community diagnostic centres, standalone clinics, or critical storage facilities. This is where unmanned building management becomes a genuinely powerful tool, but only if it’s planned correctly from day one.
In practice, unmanned building management means creating a self-sufficient, secure, and monitored environment that needs minimal hands-on intervention. It means weaving CCTV, access control, and core electrical systems into a single, cohesive ecosystem you can manage from anywhere. The promise of big savings on staffing and running costs is huge.
The trouble is, many of these projects don't quite deliver. The number one reason? A siloed approach to planning. When you design access control, power, and data networks in isolation, you end up with a fragmented, unreliable system that causes more headaches than it solves.
Designing Access, Power, and Data Together
To build a truly autonomous unit, you have to treat access, power, and data as three legs of the same stool—if one is wobbly, the whole thing comes crashing down. A high-definition CCTV camera is completely useless if the network cabling can’t handle the bandwidth or if its Power over Ethernet (PoE) feed is unstable.
This integrated design approach involves:
Unified Power Planning: Mapping out the power needs for all systems right from the start. This means calculating PoE budgets for cameras and locks, making sure there are enough outlets, and planning for an uninterruptible power supply (UPS) to keep security systems online during an outage.
Integrated Data Strategy: Designing the network to support every connected device without creating bottlenecks. This comes down to specifying the right category of structured cabling and ensuring network switches can handle the combined data load from CCTV, access logs, and environmental sensors.
Holistic Security Overlay: Making sure access control systems and CCTV actually communicate. For instance, an access attempt at a door should automatically tell the nearest camera to start recording, giving you a clear visual audit trail.
The most common failure point in unmanned building projects is underestimating the interdependence of core systems. A successful autonomous facility is not just a collection of smart devices; it's a single, integrated machine where every component is planned in relation to the others.
The Case for Battery-Less NFC Proximity Locks
One of the biggest operational headaches in unmanned facilities is maintenance, and nothing drains resources like battery-powered devices. Just imagine having to send an engineer to a remote site simply to change the batteries in a dozen door locks. It’s a massive waste of time and money.
This is exactly why battery-less, Near Field Communication (NFC) proximity locks are a game-changer for these environments. These locks are powered directly through the network cable (PoE), which gets rid of batteries completely.
Here are the real-world benefits for an NHS facilities manager:
Zero Battery Maintenance: This is the headline advantage. It completely removes the recurring cost and logistical nightmare of replacing batteries.
Enhanced Reliability: PoE provides a consistent, reliable power source. You never have to worry about a lock failing because of a dead battery, which could compromise security or lock out authorised staff.
Centralised Power Management: All power is managed from your central comms room via the network switch and can be backed up by a single UPS. This ensures every lock stays operational during a power cut.
You’ll see these systems used in places like pharmaceutical storage rooms, remote equipment shelters, and standalone community health hubs—anywhere reliability is critical and regular maintenance visits just aren't practical.
Building Out a Fully Autonomous Unit
Creating a fully autonomous unmanned building unit requires a methodical approach, and it all starts with a solid foundation of commercial electrical installation and certification. A certified electrical system is the non-negotiable first step to guaranteeing the safety and reliability of everything you connect to it.
From there, it’s about building out the integrated layers of technology. This involves deploying a structured cabling network that can support all your devices, followed by the strategic installation of CCTV cameras and access control points. With the right planning, you can achieve a truly resilient and efficient unmanned facility. For anyone looking to dig deeper into this, our guide on unmanned building management provides more technical detail.
By designing these systems as one cohesive whole from the outset, you’ll ensure long-term operational success, cut down the maintenance burden, and create a secure, reliable environment fit for modern healthcare.
Making Sure It All Works: Testing, Handover, and Long-Term Care
Let's be honest, a project isn't finished when the last cable is clipped in or the final access point is screwed to the ceiling. For an NHS facilities manager, the real moment of truth comes next. This is where we get into rigorous testing, a seamless handover to the operational teams, and a solid plan for long-term maintenance. This is the stage that proves the investment was worthwhile and ensures your new infrastructure will stand up to the demands of a busy clinical environment for years to come.
Moving from a project site buzzing with contractors to a live, operational environment needs to be a calm, methodical process. It all starts with testing – and I mean proper testing – to prove the system doesn't just switch on, but performs exactly as laid out in your technical specification. This isn't just ticking a box; it's your primary defence against the kind of performance headaches and failures that can have a real impact on patient care down the line.
Putting the New System Through Its Paces
You need to focus on two non-negotiable types of testing before you even think about signing a project off: technical certification and, just as importantly, User Acceptance Testing (UAT).
First, if you've had any new structured cabling installed, you absolutely must demand the full certification test results for every single link. Your partner should be using specialised kit like a Fluke tester to provide detailed reports that confirm each copper or fibre cable meets the standard you paid for (e.g., Cat6a). These reports measure critical metrics like insertion loss and crosstalk, giving you undeniable proof of a quality installation that won't let you down.
Don't just settle for a summary sheet. Insist on seeing the individual test results for every single cable. This paperwork is your leverage and is absolutely essential if you ever need to call on that 25-year manufacturer warranty.
Next up is User Acceptance Testing (UAT), which means getting the people who will actually use the system—your clinical staff—to try and break it. This isn't about the tech specs; it's about seeing if it works in the real world, under pressure.
Simulate a Ward Round: Get a nurse to log into the EPR system on a mobile workstation and walk the full length of the ward. Does the Wi-Fi connection roam seamlessly, or does it drop out?
Test High-Demand Scenarios: Ask several clinicians in the new area to pull up large imaging files at the same time. Does the network grind to a halt or handle the load?
Check Device Compatibility: Connect a mix of the typical medical devices you use every day. Do they all connect to the network quickly and communicate without any frustrating lag?
By getting your end-users involved, you not only confirm the system is fit for purpose but you also build their confidence in it from day one.
The Handover: From Project Team to Your Team
A smooth handover is all about the quality of the documentation. When the project is finally signed off, your implementation partner must provide a complete handover pack. Think of this as the operational bible for your new system.
A proper handover pack should always contain:
As-Built Drawings: Not the plans, but detailed diagrams showing the actual final location of all cabling, outlets, cabinets, and hardware.
Full Asset Register: A complete inventory of everything installed, right down to the serial numbers, models, and warranty details.
Configuration Files: A backup of the final settings for every network switch, access point, and firewall.
Warranty Certificates: The official documents for all hardware and, crucially, the 25-year cabling system warranty.
Support and Escalation Contacts: Clear instructions for your in-house estates and IT teams on day-to-day management, plus a defined contact list for support issues.
Planning for Life After Go-Live
Your job as an NHS facilities manager doesn't stop when the contractors leave site. To get the most out of this investment, you need a clear plan for ongoing maintenance and support. This means knowing exactly what the warranties cover and having a Service Level Agreement (SLA) in place for when things go wrong.
Map out who is responsible for what. Your in-house team might handle first-line troubleshooting, while your external partner provides the expert support for complex hardware failures or configuration problems. Knowing exactly who to call and the response time you can expect is what minimises downtime and ensures this new infrastructure remains the reliable foundation for patient care you intended it to be.
Your Questions Answered: An NHS Facilities Manager's Guide
Even the most meticulously planned IT infrastructure project will throw up challenges. When you're managing complex upgrades within the NHS, having solid answers ready for the tough questions is essential. Here are our straight-talking answers to the most common queries we get from facilities managers on the ground.
How Do I Justify the Budget for a Major Cabling Upgrade?
The key is to frame the project as an investment in clinical resilience and risk mitigation, not just another IT expense. An unreliable or outdated network has a direct, measurable impact on patient care. It causes delays in accessing electronic health records and creates unstable connections for critical medical equipment.
Build your business case with hard data. Use specific figures on clinical service incidents that were caused by failures in the estate's infrastructure. A modern, certified network isn’t a cost centre; it's a foundational investment that reduces long-term maintenance headaches and enables the digital health initiatives of the future.
What Are the Most Common Points of Failure in These Projects?
From our experience, projects most often stumble in two areas: inadequate planning and poor communication with stakeholders. A project can look perfect on paper but cause chaos if the team doesn't fully grasp the clinical workflows it's supposed to support. This leads to solutions that are technically brilliant but operationally disruptive.
The other major pitfall is underestimating the sheer complexity of working inside a live hospital. That means failing to coordinate properly with infection control, not planning for unavoidable out-of-hours work, or simply not having a technical specification that’s detailed enough on future scalability and security.
What Should I Look for in an External IT Infrastructure Partner?
You need a partner with specific, demonstrable experience inside the NHS. Don't be afraid to ask for case studies—specifically, projects that demanded minimal downtime and involved meticulously planned, staged migrations in live clinical environments.
Check their technical certifications, but just as importantly, ensure they offer a manufacturer-backed 25-year warranty for their cabling work, as this is the industry standard. The biggest differentiator, though, is their process. A great partner works collaboratively with your in-house teams from day one and has integrated expertise across networking, electrical, and compliance. They need to provide a true end-to-end solution.
The right partner doesn't just install equipment; they understand the clinical context. Their ability to speak the language of both IT and healthcare is what separates a successful project from a disruptive one.
How Do We Ensure New CCTV and Access Control Systems Are Integrated Effectively?
Effective integration has to be designed in from the very beginning—it can't be bolted on as an afterthought. During the specification phase, you need to be crystal clear about the bandwidth demands, Power over Ethernet (PoE) budgets, and network security policies for these systems.
Your partner must conduct a thorough survey of the existing network to confirm it can handle the extra data load without impacting performance. The project plan should also detail how these new systems will be properly segmented (using VLANs, for example) to guarantee both security and operational integrity. A successful integration depends on designing access, power, and data as one cohesive system.
At Constructive-IT, we have over 20 years of experience delivering end-to-end IT and network infrastructure projects for demanding environments like the NHS. From initial planning and stakeholder engagement to certified installation and on-site go-live support, we provide the specialist expertise to ensure your project succeeds without disrupting critical services.
To discuss your next project with an expert, get in touch with our team.






Comments